REKOMENDACJE DOTYCZĄCE POSTĘPOWANIA
W ZAKAŻENIACH MĘSKIEGO UKŁADU
MOCZOWEGO I PŁCIOWEGO
GUIDELINES ON UROLOGICAL INFECTIONS
G. Bonkat (przewodniczący), R.R. Bartoletti, F. Bruyère, T. Cai, S.E. Geerlings, B. Köves, S. Schubert,
F. Wagenlehner, Mezei, A. Pilatz, B. Pradere, R. Veeratterapillay
Tłumaczenie i przygotowanie wersji polskiej / Translation and elaboration of Polish version:
Marta Sochaj1, Jolanta Słowikowska-Hilczer2
Katedra Humanizacji Medycyny i Seksuologii, Uniwersytet Zielonogórski; 2 Zakład Endokrynologii Płodności, Katedra Andrologii
i Endokrynologii Płodności, Uniwersytet Medyczny w Łodzi
Autor do korespondencji / corresponding author:
Jolanta Słowikowska-Hilczer, Zakład Endokrynologii Płodności, Katedra Andrologii i Endokrynologii Płodności, Uniwersytet Medyczny
w Łodzi, ul. Pomorska 251. 92-213 Łódź, tel.: 42 201-41-42, jolanta.slowikowska-hilczer@umed.lodz.pl
Otrzymano/received: 25.11.2019 r. Zaakceptowano/accepted: 27.12.2019 r.
DOI: 10.26404/PAO_2353-8791.2019.08
Skróty / Abbreviations
i.m. – domięśniowo (łac. iniectio intramuscularis); LE – poziom wiarygodności dowodu naukowego (ang. level of evidence); PCR – łańcuchowa
reakcja polimerazy (ang. polymeras chain reaction); p.o. – doustnie (łac. per os); PSA – swoisty antygen prostaty (ang. prostate specific antigen)
Piśmiennictwo
strong>Piśmiennictwo
Abbara A., Davidson R.N.: Etiology and management of genitourinary tuberculosis. Nat Rev Urol. 2011, 8 (12), 678–688. doi: 10.1038/nrurol.2011.172.
https://www.ncbi.nlm.nih.gov/pubmed/22157940
Abrutyn E., Berlin J., Mossey J., Pitsakis P., Levison M., Kaye D.: Does treatment of asymptomatic bacteriuria in older ambulatory women reduce subsequent symptoms of urinary tract infection? J Am Geriatr Soc. 1996, 44
(3), 293–295. doi: 10.1111/j.1532-5415.1996.tb00917.x https://www.ncbi.
nlm.nih.gov/pubmed/8600199
Abrutyn E., Mossey J., Berlin J.A., Boscia J., Levison M., Pitsakis P. i wsp.: Does
asymptomatic bacteriuria predict mortality and does antimicrobial treatment reduce mortality in elderly ambulatory women? Ann Intern Med.
1994, 120 (10), 827–833. doi: 10.7326/0003-4819-120-10-199405150-
00003. https://www.ncbi.nlm.nih.gov/pubmed/7818631
Abughosh Z., Margolick J., Goldenberg S.L., Taylor S.A., Afshar K., Bell R i wsp.:
A prospective randomized trial of povidone-iodine prophylactic cleansing
of the rectum before transrectal ultrasound guided prostate biopsy. J Urol.
2013, 189 (4), 1326–1331. doi: 10.1016/j.juro.2012.09.121. https://www.
ncbi.nlm.nih.gov/pubmed/23041343
Albert X., Huertas I., Pereiró I.I., Sanfélix J., Gosalbes V., Perrota C.: Antibiotics
for preventing recurrent urinary tract infection in non-pregnant women.
Cochrane Database Syst Rev. 2004, CD001209. doi: 10.1002/14651858.
CD001209.pub2. https://www.ncbi.nlm.nih.gov/pubmed/15266443
Alexander R.B., Ponniah S., Hasday J., Hebel J.R.: Elevated levels of proinflammatory cytokines in the semen of patients with chronic prostatitis/
chronic pelvic pain syndrome. Urology. 1998, 52 (2), 744–749. doi: 10.1016/
s0090-4295(98)00390-2. https://www.ncbi.nlm.nih.gov/pubmed/9801092
Alexander R.B., Trissel D.: Chronic prostatitis: results of an Internet survey.
Urology. 1996, 48 (4), 568–574. doi: 10.1016/s0090-4295(96)00234-8.
https://www.ncbi.nlm.nih.gov/pubmed/8886062
Aliaev Iu G., Vinarov A.Z., Akhvlediani N.D.: [Wardenafil in combined treatment of patients with chronic bacterial prostatitis]. Urologiia. 2008, 52–55.
https://www.ncbi.nlm.nih.gov/pubmed/19256057
Andersen B., van Valkengoed I., Sokolowski I., Møller J.K., Østergaard L., Olesen
F.: Impact of intensified testing for urogenital Chlamydia trachomatis infections: a randomised study with 9-year follow-up. Sex Transm Infect. 2011,
87 (2), 156–161. doi: 10.1136/sti.2010.042192. https://www.ncbi.nlm.nih.
gov/pubmed/21097811
Angeletti S., Dicuonzo G., Fioravanti M., De Cesaris M., Fogolari M., Lo Presti A.
i wsp.: Procalcitonin, MR-Proadrenomedullin, and Cytokines Measurement
in Sepsis Diagnosis: Advantages from Test Combination. Dis Markers. 2015,
2015: 951532. doi: 10.1155/2015/951532. https://www.ncbi.nlm.nih.gov/
pubmed/26635427
Antibacterial prophylaxis in surgery: 2 - Urogenital, obstetric and gynaecological surgery. Drug Ther Bull. 2004, 42, 9. https://www.ncbi.nlm.nih.
gov/pubmed/15067952
Arnold A., Aitchison L.P., Abbott J.: Preoperative Mechanical Bowel
Preparation for Abdominal, Laparoscopic, and Vaginal Surgery: A Systematic
Review. J Minim Invasive Gynecol. 2015, 22 (5), 737–752. doi: 10.1016/j.
jmig.2015.04.003. https://www.ncbi.nlm.nih.gov/pubmed/25881881
Aron M., Rajeev T.P., Gupta N.P.: Antibiotic prophylaxis for transrectal needle biopsy of the prostate: A randomized controlled study. BJU Int. 2000,
85 (6), 682–985. doi: 10.1046/j.1464-410x.2000.00576.x. https://www.
ncbi.nlm.nih.gov/pubmed/10759665
Asscher A.W., Sussman M., Waters W.E., Evans J.A., Campbell H., Evans K.T.
i wsp.: The clinical significance of asymptomatic bacteriuria in the nonpregnant woman. J Infect Dis. 1969, 120 (1), 17–26. doi: 10.1093/infdis/120.1.17.
https://www.ncbi.nlm.nih.gov/pubmed/5803281
Badalyan R.R., Fanarjyan S.V., Aghajanyan I.G.: Chlamydial and ureaplasmal
infections in patients with nonbacterial chronic prostatitis. Andrologia.
2003, 35 (5), 263–265. https://www.ncbi.nlm.nih.gov/pubmed/14535852
Bader M.S., Hawboldt J., Brooks A.: Management of complicated urinary
tract infections in the era of antimicrobial resistance. Postgrad Med. 2010,
122 (6), 7–15. doi: 10.3810/pgm.2010.11.2217. https://www.ncbi.nlm.nih.
gov/pubmed/21084776
Bailey R.R., Bishop V., Peddie B.A.: Comparison of single dose with a 5-day
course of co-trimoxazole for asymptomatic (covert) bacteriuria of pregnancy.
Aust N Z J Obstet Gynaecol. 1983, 23 (3), 139–141. doi: 10.1111/j.1479-
-828x.1983.tb00562.x. https://www.ncbi.nlm.nih.gov/pubmed/6606421
Banyra O., Shulyk A.: Acute epididymo-orchitis: staging and treatment. Cent
Eur J Urol. 2012, 65 (3), 139–143. doi: 10.5173/ceju.2012.03.art8. https://
www.ncbi.nlm.nih.gov/pubmed/24578950
Bauer H.W., Alloussi S., Egger G., Blümlein H.M., Cozma G., Schulman C.C.: A
long-term, multicenter, double-blind study of an Escherichia coli extract
(OM-89) in female patients with recurrent urinary tract infections. Eur
Urol. 2005, 47 (4), 542–548. doi: 10.1016/j.eururo.2004.12.009. https://
www.ncbi.nlm.nih.gov/pubmed/15774256.
Bauer H.W., Rahlfs V.W., Lauener P.A., Blessmann G.S.: Prevention of recurrent
urinary tract infections with immuno-active E. coli fractions: a meta-analysis of five placebo-controlled double-blind studies. Int J Antimicrob Agents.
2002, 19 (6), 451–456. https://www.ncbi.nlm.nih.gov/pubmed/12135831
Bayrak O., Cimentepe E., Inegöl I., Atmaca A.F., Duvan C.I., Koç A. i wsp.: Is
single-dose fosfomycin trometamol a good alternative for asymptomatic
bacteriuria in the second trimester of pregnancy? Int Urogynecol J Pelvic
Floor Dysfunct. 2007, 18 (5), 525–529. doi: 10.1007/s00192-006-0190-y.
https://www.ncbi.nlm.nih.gov/pubmed/16941068
Beerepoot M.A., Geerlings S.E., van Haarst E.P., van Charante N.M., ter Riet
G.: Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol.
2013, 190 (6), 1981–1989. doi: 10.1016/j.juro.2013.04.142. https://www.
ncbi.nlm.nih.gov/pubmed/23867306
Bell B.G., Schellevis F., Stobberingh E., Goossens H., Pringle M.: A systematic
review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014, 14, 13. doi: 10.1186/1471-2334-
14-13. https://www.ncbi.nlm.nih.gov/pubmed/24405683
Bent S., Nallamothu B.K., Simel D.L., Fihn S.D., Saint S.: Does this woman
have an acute uncomplicated urinary tract infection? JAMA. 2002, 287
(20), 2701–2710. doi: 10.1001/jama.287.20.2701. https://www.ncbi.nlm.
nih.gov/pubmed/12020306
Berger R.E.: Epididymitis. W: Red. K.K. Holmes, P.A. Mardh, P.F. Sparling,
P.J. Wiesner. Sexually transmitted diseases. McGraw-Hill, New York 1984.
Bint A., Bullock D., Reeves D., Wilkinson P.: A comparative trial of pivmecillinam
and ampicillin in bacteriuria of pregnancy. Infection. 1979, 7 (6), 290–293.
doi: 10.1007/bf01642151. https://www.ncbi.nlm.nih.gov/pubmed/232697
Bjerklund Johansen T.E., Grüneberg R.N., Guibert J., Hofstetter A., Lobel B., Naber
K.G. i wsp.: The role of antibiotics in the treatment of chronic prostatitis: a consensus statement. Eur Urol. 1998, 34 (6), 457–466. doi: 10.1159/000019784.
https://www.ncbi.nlm.nih.gov/pubmed/9831786
Blok B., Castro-Diaz D., Del Popolo G., Groen J., Hamid R., Karsenty G. i wsp.:
EAU Guidelines on Neuro-urology. In: EAU Guidelines, edition presented
at the annual EAU Congress Barcelona 2019. ISBN 978-94-92671-04-2.
https://uroweb.org/guideline/neuro-urology/
Bone R.C., Balk R.A., Cerra F.B., Dellinger R.P., Fein A.M., Knaus W.A. i wsp.:
Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee.
American College of Chest Physicians/Society of Critical Care Medicine.
Chest. 1992, 101 (6), 1644–1655. doi: 10.1378/chest.101.6.1644. https://
www.ncbi.nlm.nih.gov/pubmed/1303622
Bonkat G., Braissant O., Cai T., Köves B., Bjerklund Johansen T.E., Pickard R.
i wsp.: Non-molecular Methods to Detect Bacteriuria Prior to Urological
Interventions: A Diagnostic Accuracy Systematic Review. Eur Urol Focus.
2017, 3 (6), 535–537. doi: 10.1016/j.euf.2018.03.004. https://www.ncbi.
nlm.nih.gov/pubmed/29627196
Bonkat G., Pickard R., Bartoletti R., Cai T., Bruyère F., Geerlings S.E. i wsp.: EAU
Guidelines on Urological Infection. In: EAU Guidelines, edition presented
at the annual EAU Congress Copenhagen 2018. ISBN 978-94-92671-01-1.
Bonkat G., Widmer A.F., Rieken M., van der Merwe A., Braissant O., Müller
G. i wsp.: Microbial biofilm formation and catheter-associated bacteriuria
in patients with suprapubic catheterisation. World J Urol. 2013, 31 (3),
565–571. doi: 10.1007/s00345-012-0930-1. https://www.ncbi.nlm.nih.
gov/pubmed/22926265
Bootsma A.M.J., Laguna Pes M.P., Geerlings S.E., Goossens A.: Antibiotic
Prophylaxis in Urologic Procedures: A Systematic Review. Eur Urol. 2008,
54 (6), 1270–1286. doi: 10.1016/j.eururo.2008.03.033. https://www.ncbi.
nlm.nih.gov/pubmed/50098356
Borchardt K.A., al-Haraci S., Maida N.: Prevalence of Trichomonas vaginalis
in a male sexually transmitted disease clinic population by interview, wet
mount microscopy, and the InPouch TV test. Genitourin Med. 1995, 71
(6), 405–406. doi: 10.1136/sti.71.6.405. https://www.ncbi.nlm.nih.gov/
pubmed/8566985
Boscia J.A., Kobasa W.D., Knight R.A., Abrutyn E., Levison M.E., Kaye D.:
Therapy vs no therapy for bacteriuria in elderly ambulatory nonhospitalized women. JAMA. 1987, 257 (8), 1067–1071. https://www.ncbi.nlm.nih.
gov/pubmed/3806896
Bradbury S.M.: Collection of urine specimens in general practice: to clean
or not to clean? J R Coll Gen Pract. 1988, 38, 363–365. https://www.ncbi.
nlm.nih.gov/pubmed/3256648
Bremer V., Buder N., Eigentler A>, Esser S., Hagedorn H.J., Hartmann M. i wsp.:
Gonorrhoea in adults and adolescents AWMF S2k guidelines. 2013. Nr.
059/004. http://www.egms.de/static/en/journals/id/2014-2/id000010.shtml
Brown R.W., Warner J.J., Turner B.I., Harris L.F., Alford R.H.: Bacteremia
and bacteriuria after transrectal prostatic biopsy. Urology. 1981, 18 (2),
145–148. doi: 10.1016/0090-4295(81)90425-8. https://www.ncbi.nlm.
nih.gov/pubmed/7269016
Brun-Buisson C., Meshaka P., Pinton P., Vallet B.: EPISEPSIS: a reappraisal of
the epidemiology and outcome of severe sepsis in French intensive care
units. Intensive Care Med. 2004, 30 (4), 580–588. doi: 10.1007/s00134-
003-2121-4. https://www.ncbi.nlm.nih.gov/pubmed/14997295
Brunkhorst F.M., Wegscheider K., Forycki Z.F., Brunkhorst R.: Procalcitonin for
early diagnosis and differentiation of SIRS, sepsis, severe sepsis, and septic shock. Intensive Care Med. 2000, 26 Suppl 2, S148–S152. doi: 10.1007/
BF02900728. https://www.ncbi.nlm.nih.gov/pubmed/18470710
Budia A., Luis Palmero J., Broseta E., Tejadillos S., Benedicto A., Queipo J.A.
i wsp.: Value of semen culture in the diagnosis of chronic bacterial prostatitis: a simplified method. Scand J Urol Nephrol. 2006, 40 (4), 326–
331. doi: 10.1080/00365590600748247. https://www.ncbi.nlm.nih.gov/
pubmed/16916775
Busolo F., Camposampiero D., Bordignon G., Bertollo G.: Detection of Mycoplasma
genitalium and Chlamydia trachomatis DNAs in male patients with urethritis using the polymerase chain reaction. New Microbiol. 1997, 20 (4),
325–332. https://www.ncbi.nlm.nih.gov/pubmed/9385602
Cafferkey M.T., Falkiner F.R., Gillespie W.A., Murphy D.M.: Antibiotics for
the prevention of septicaemia in urology. J Antimicrob Chemother. 1982,
9 (6), 471–477. doi: 10.1093/jac/9.6.471. https://www.ncbi.nlm.nih.gov/
pubmed/7107549
Cai T., Mazzoli S., Addonisio P., Boddi V., Geppetti P., Bartoletti R.: Clinical and
microbiological efficacy of prulifloxacin for the treatment of chronic bacterial
prostatitis due to Chlamydia trachomatis infection: results from a prospective, randomized and open-label study. Methods Find Exp Clin Pharmacol.
2010, 32 (1), 39–45. doi: 10.1358/mf.2010.32.1.1423885. https://www.
ncbi.nlm.nih.gov/pubmed/20383345
Cai T., Mazzoli S., Bechi A., Addonisio P., Mondaini N., Pagliai R.C. i wsp.: Serenoa
repens associated with Urtica dioica (ProstaMEV) and curcumin and quercitin (FlogMEV) extracts are able to improve the efficacy of prulifloxacin in
bacterial prostatitis patients: results from a prospective randomised study.
Int J Antimicrob Agents. 2009, 33 (6), 549–593. doi: 10.1016/j.ijantimicag.2008.11.012. https://www.ncbi.nlm.nih.gov/pubmed/19181486
Cai T., Mazzoli S., Mondaini N., Meacci F., Nesi G., D’Elia C. i wsp.: The role of
asymptomatic bacteriuria in young women with recurrent urinary tract
infections: To treat or not to treat? Clin Infect Dis. 2012, 55 (6), 771–777.
doi: 10.1093/cid/cis534. https://www.ncbi.nlm.nih.gov/pubmed/22677710
Cam K., Kayikci A., Akman Y., Erol A.: Prospective assessment of the efficacy of single dose versus traditional 3-day antimicrobial prophylaxis in
12-core transrectal prostate biopsy. Int J Urol. 1001, 15 (11), 997–1001.
doi: 10.1111/j.1442-2042.2008.02147.x. https://www.ncbi.nlm.nih.gov/
pubmed/18721198
Campbell-Brown M., McFadyen I.R., Seal D.V., Stephenson M.L.: Is screening
for bacteriuria in pregnancy worth while? Br Med J (Clin Res Ed). 1987,
294, 1579–1582. doi: 10.1136/bmj.294.6587.1579. https://www.ncbi.nlm.
nih.gov/pubmed/3113538
Carey M.M., Zreik A., Fenn N.J., Chlosta P.L., Aboumarzouk O.M.: Should We
Use Antibiotic Prophylaxis for Flexible Cystoscopy? A Systematic Review and
Meta-Analysis. Urol Int. 2015, 95 (3), 249–259. doi: 10.1159/000381882.
https://www.ncbi.nlm.nih.gov/pubmed/26138144
Carlet J., Dumay M.F., Gottot S.: Guidelines for prevention of nosocomial
infections in intensive care unit. Arnette Ed Paris 1994, 41.
Caskurlu T., Arikan O., Yildrim A., Tanidir B., Canakci C., Danacioglu Y.A. i wsp.:
MP48-01 Prevalence of antibiotic resistance in fecal flora before transrectal
ultrasound-guided prostate biopsy and clinical impact of targeted antibiotic prophylaxis. J Urol. 2015, 193, e594. https://www.jurology.com/doi/
pdf/10.1016/j.juro.2015.02.1675
Cefai C., Charani E., Craven L.: Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use. NICE Guidelines, 2015.
https://www.nice.org.uk/guidance/ng15
Cek M., Tandoğdu Z., Wagenlehner F., Tenke P., Naber K., Bjerklund-Johansen
T.E.: Healthcare-associated urinary tract infections in hospitalized urological patients – a global perspective: results from the GPIU studies 2003-2010.
World J Urol. 2014, 32 (6), 1587–1594. doi: 10.1007/s00345-013-1218-9.
https://www.ncbi.nlm.nih.gov/pubmed/24452449
Centers for Disease Control and Prevention. 2015 Sexually Transmitted
Diseases Treatment Guidelines – Epididymitis. 2015. https://www.cdc.
gov/std/tg2015/epididymitis.htm
Centers for Disease Control and Prevention. Procedure-associated Module
9: Surgical Site Infection (SSI) Event. 2017. https://www.cdc.gov/nhsn/pdfs/
pscmanual/9pscssicurrent.pdf
Chae Y., Kim Y.J., Kim T., Yun S.J., Lee S.C., Kim W.J.: The Comparison between
Transperineal and Transrectal Ultrasound-Guided Prostate Needle Biopsy.
Korean J Urol. 2009, 50 (2), 119–124. doi: 10.4111/kju.2009.50.2.119. https://
synapse.koreamed.org/Synapse/Data/PDFData/0020KJU/kju-50-119.pdf
Chazan B., Zelichenko G., Shental Y., Edelstein H., Raz R.: Antimicrobial prophylaxis for transrectal ultrasound guided biopsy of prostate: A comparative
study between single dose of Gentamicin vs. Ofloxacin. Int J Inf Dis. 2010,
14, Suppl 1, 199–200. doi: 10.1016/j.ijid.2010.02.1930. https://www.ijidonline.com/article/S1201-9712(10)01970-3/fulltext
Chennamsetty A., Khourdaji I., Burks F., Killinger K.A.: Contemporary diagnosis and management of Fournier’s gangrene. Ther Adv Urol. 2015, 7 (4),
203–215. doi: 10.1177/1756287215584740. https://www.ncbi.nlm.nih.
gov/pubmed/26445600
Chong J.T., Klausner A.P., Petrossian A., Byrne M.D., Moore J.R., Goetz L.L.
i wsp.: Pre-procedural antibiotics for endoscopic urological procedures:
Initial experience in individuals with spinal cord injury and asymptomatic bacteriuria. J Spinal Cord Med. 2015, 38 (2), 187–192. doi:
10.1179/2045772313Y.0000000185. https://www.ncbi.nlm.nih.gov/
pubmed/24621035
Chou Y.H., Tiu C.M., Liu J.Y., Chen J.D., Chiou H.J., Chiou S.Y. i wsp.: Prostatic
abscess: transrectal color Doppler ultrasonic diagnosis and minimally invasive therapeutic management. Ultrasound Med Biol. 2004, 30 (6), 719–724.
doi: 10.1016/j.ultrasmedbio.2004.03.014. https://www.ncbi.nlm.nih.gov/
pubmed/15219951
Christopher L.J., Thompson G.R.: A trial of hippramine in the treatment of
bacteriuria of pregnancy. Ir J Med Sci. 1969, 8 (7), 331–337. doi: 10.1007/
bf02955410. https://www.ncbi.nlm.nih.gov/pubmed/5806178
Classen D.C., Larsen R.A., Burke J.P., Stevens L.E.: Prevention of catheter-associated bacteriuria: clinical trial of methods to block three known pathways
of infection. Am J Infect Control. 1991, 19 (3), 136–142. doi: 10.1016/0196-
6553(91)90019-9. https://www.ncbi.nlm.nih.gov/pubmed/1863002
Cooper F.P., Alexander C.E., Sinha S., Omar M.I.: Policies for replacing longterm indwelling urinary catheters in adults. Cochrane Database Syst Rev.
2016, 7, CD011115. doi: 10.1002/14651858.CD011115.pub2. https://www.
ncbi.nlm.nih.gov/pubmed/27457774
Cordero-Ampuero J., González-Fernández E., Martínez-Vélez D., Esteban J.: Are
antibiotics necessary in hip arthroplasty with asymptomatic bacteriuria?
Seeding risk with/without treatment. Clin Orthop Relat Res. 2013, 471
(12), 3822–3829. doi: 10.1007/s11999-013-2868-z. https://www.ncbi.nlm.
nih.gov/pubmed/23430723
Cormio L., Berardi B., Callea A., Fiorentino N., Sblendorio D., Zizzi V. i wsp.:
T Antimicrobial prophylaxis for transrectal prostatic biopsy: A prospective study of ciprofloxacin vs piperacillin/tazobactam. BJU Int. 2002, 90
(7), 700–702. doi: 10.1046/j.1464-410x.2002.02991.x. https://www.ncbi.
nlm.nih.gov/pubmed/12410751
Çek M., Sturdza L., Pilatz A.: Acute and Chronic Epididymitis in EAU-EBU
Update Series. Eur Urol Suppl 2017. 16: 124. https://www.sciencedirectcom/
journal/european-urology-supplements/vol/16/issue/4
Dadashpour M., Bagheri S.M.: Acute Prostatitis After Transrectal Ultrasoundguided Prostate Biopsy: Comparing Two Different Antibiotic Prophylaxis
Regimen. Biomed Pharmacol J. 2016, 9 (2), 593–597. doi: 10.13005/bpj/977.
http://biomedpharmajournal.org/vol9no2/acute-prostatitis/
Dahm P., Dmochowski R.: Evidence-based Urology. BMJ Books, London
2010, 50.
Damiano R., Quarto G., Bava I., Ucciero G., De Domenico R., Palumbo M.I.
i wsp.: Prevention of recurrent urinary tract infections by intravesical
administration of hyaluronic acid and chondroitin sulphate: a placebo-controlled randomised trial. Eur Urol. 2011, 59 (4), 645–651. doi: 10.1016/j.
eururo.2010.12.039. https://www.ncbi.nlm.nih.gov/pubmed/21272992
Darouiche R.O., Thornby J.I., Cerra-Stewart C., Donovan W.H., Hull R.A.:
Bacterial interference for prevention of urinary tract infection: a prospective, randomized, placebo-controlled, double-blind pilot trial. Clin Infect
Dis. 2005, 41 (10), 1531–1534. doi: 10.1086/497272. https://www.ncbi.
nlm.nih.gov/pubmed/16231269
Dasgupta R., Grabe M.: Preoperative antibiotics before endourologic surgery: current recommendations. J Endourol. 2009, 23 (10), 1567–1570. doi:
10.1089/end.2009.1520. https://www.ncbi.nlm.nih.gov/pubmed/19785548
Davey P., Brown E., Charani E., Fenelon L., Gould I.M., Holmes A. i wsp.:
Interventions to improve antibiotic prescribing practices for hospital inpatients.
Cochrane Database Syst Rev. 2013, 4: CD003543. doi: 10.1002/14651858.
CD003543.pub3. https://www.ncbi.nlm.nih.gov/pubmed/23633313
DeGroot-Kosolcharoen J., Guse R., Jones J.M.: Evaluation of a urinary catheter
with a preconnected closed drainage bag. Infect Control Hosp Epidemiol.
1988, 9 (2), 72–76. doi: 10.1086/645788. https://www.ncbi.nlm.nih.gov/
pubmed/3343502
Dellinger R.P., Carlet J.M., Masur H., Gerlach H., Calandra T., Cohen J. i wsp.:
Surviving Sepsis Campaign guidelines for management of severe sepsis
and septic shock. Crit Care Med. 2004, 32 (3), 858–873. doi: 10.1097/01.
ccm.0000117317.18092.e4. https://www.ncbi.nlm.nih.gov/pubmed/15090974
Dellinger R.P., Levy M.M., Rhodes A., Annane D., Gerlach H., Opal S.M. i wsp.:
Surviving Sepsis Campaign: international guidelines for management of
severe sepsis and septic shock, 2012. Intensive Care Med. 2013, 39 (2),
165–228. doi: 10.1007/s00134-012-2769-8. https://www.ncbi.nlm.nih.
gov/pubmed/23361625
Dellit T.H., Owens R.C., McGowan J.E. Jr, Gerding D.N., Weinstein R.A., Burke J.P.
i wsp.: Infectious Diseases Society of America and the Society for Healthcare
Epidemiology of America guidelines for developing an institutional program
to enhance antimicrobial stewardship. Clin Infect Dis. 2007, 44 (2), 159–177.
doi: 10.1086/510393. https://www.ncbi.nlm.nih.gov/pubmed/17173212
Del Rio C., Hall G., Holmes K., Soge O., Hook E., Kirkcaldy R. i wsp.: Update to
CDC’s Sexually Transmitted Diseases Treatment Guidelines, 2010: Oral
cephalosporins no longer a recommended treatment for gonococcal infections. MMWR Morb Mortal Wkly Rep. 2012, 61, 590–594. https://www.
ncbi.nlm.nih.gov/pubmed/22874837
Doble A., Carter S.S.: Ultrasonographic findings in prostatitis. Urol Clin North
Am. 1989, 16 (4), 763–772. https://www.ncbi.nlm.nih.gov/pubmed/2683305
Dumville J.C., McFarlane E., Edwards P., Lipp A., Holmes A., Liu Z.: Preoperative
skin antiseptics for preventing surgical wound infections after clean surgery.
Cochrane Database Syst Rev, 2015: CD003949. doi: 10.1002/14651858.
CD003949.pub4. https://www.ncbi.nlm.nih.gov/pubmed/25897764
Eickhoff J.H., Frimodt-Møller N., Walter S., Frimodt-Møller C.A.: doubleblind, randomized, controlled multicentre study to compare the efficacy
of ciprofloxacin with pivampicillin as oral therapy for epididymitis in men
over 40 years of age. BJU Int. 1999, 84 (7), 827–834. doi: 10.1046/j.1464-
410x.1999.00252.x. https://www.ncbi.nlm.nih.gov/pubmed/10532980
Eke N.: Fournier’s gangrene: a review of 1726 cases. Br J Surg. 2000, 87 (6),
718–728. doi: 10.1046/j.1365-2168.2000.01497.x. https://www.ncbi.nlm.
nih.gov/pubmed/10848848
El Amari E.B., Hadaya K., Bühler L., Berney T., Rohner P., Martin P.Y. i wsp.:
Outcome of treated and untreated asymptomatic bacteriuria in renal transplant recipients. Nephrol Dial Transplant. 2011, 26 (12), 4109–4114. doi:
10.1093/ndt/gfr198. https://www.ncbi.nlm.nih.gov/pubmed/21592976
Elder H.A., Santamarina B.A., Smith S., Kass E.H.: The natural history of
asymptomatic bacteriuria during pregnancy: the effect of tetracycline on
the clinical course and the outcome of pregnancy. Am J Obstet Gynecol.
1971, 111 (3), 441–462. doi: 10.1016/0002-9378(71)90793-9. https://www.
ncbi.nlm.nih.gov/pubmed/4937729
Elder H.A., Santamarina B.A., Smith S.A., Kass E.H.: Use of sulfasymazine in the treatment of bacteriuria of pregnancy. Antimicrob Agents
Chemother (Bethesda). 1966, 6, 142–148. https://www.ncbi.nlm.nih.gov/
pubmed/4862162
Estebanez A., Pascual R., Gil V., Ortiz F., Santibáñez M., Pérez Barba C.:
Fosfomycin in a single dose versus a 7-day course of amoxicillin- clavulanate for the treatment of asymptomatic bacteriuria during pregnancy.
Eur J Clin Microbiol Infect Dis. 2009, 28 (12), 1457–1464. doi: 10.1007/
s10096-009-0805-6. https://www.ncbi.nlm.nih.gov/pubmed/19768649
Etienne M., Pestel-Caron M., Chavanet P., Caron F.: Performance of the urine
leukocyte esterase and nitrite dipstick test for the diagnosis of acute prostatitis. Clin Infect Dis. 2008, 46 (6), 951–953. doi: 10.1086/528873. https://
www.ncbi.nlm.nih.gov/pubmed/18288905
European Centre for Disease Prevention and Control (ECDC). Systematic
review and evidence-based guidance on perioperative antibiotic prophylaxis. 2013. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/Perioperative%20antibiotic%20prophylaxis%20-%20
June%202013.pdf
European Centre for Disease Prevention and Control. Annual Epidemiological
Report 2016 – Healthcare-associated infections acquired in intensive care
units. 2016. https://ecdc.europa.eu/en/publications-data/healthcare-associated-infections-intensive-care-units-annual-epidemiological-0
Evans B.A., Bond R.A., MacRae K.D.: Racial origin, sexual behaviour, and
genital infection among heterosexual men attending a genitourinary medicine clinic in London (1993-4). Sex Transm Infect. 1998, 74 (1), 40–44.
doi: 10.1136/sti.74.1.40. https://www.ncbi.nlm.nih.gov/pubmed/9634302
Falagas M.E., Kotsantis I.K., Vouloumanou E.K., Rafailidis P.I.: Antibiotics
versus placebo in the treatment of women with uncomplicated cystitis:
a meta-analysis of randomized controlled trials. J Infect. 2009, 58 (2),
91–102. doi: 10.1016/j.jinf.2008.12.009. https://www.ncbi.nlm.nih.gov/
pubmed/19195714
Fang Y.Q., Li T.C., Si T.J., Pang J., Gao X.: Antibiotic prophylaxis at time of
catheter removal following laparoscopic radical prostatectomy: A prospective randomized study. Acta Medica Mediterranea. 2014, 30, 161. http://
www.actamedicamediterranea.com/archive/2014/medica-1/antibioticprophylaxis-at-time-of-catheter-removal-following-laparoscopic-radicalprostatectomy-a-prospective-randomized-study
Fihn S.D.: Clinical practice. Acute uncomplicated urinary tract infection in
women. N Engl J Med. 2003, 349 (3), 259–266. doi: 10.1056/NEJMcp030027.
https://www.ncbi.nlm.nih.gov/pubmed/12867610
Foon R., Toozs-Hobson P., Latthe P.: Prophylactic antibiotics to reduce the
risk of urinary tract infections after urodynamic studies [Systematic
Review]. Cochrane Database of Systematic Reviews. 2012. 10: 10. doi:
10.1002/14651858.CD008224.pub2. https://www.ncbi.nlm.nih.gov/
pubmed/23076941
Foxman B.: Epidemiology of urinary tract infections: incidence, morbidity,
and economic costs. Dis Mon. 2003, 49 (2), 53–70. doi: 10.1067/mda.2003.7.
https://www.ncbi.nlm.nih.gov/pubmed/12601337
Foxman B.: Epidemiology of urinary tract infections: transmission and risk
factors, incidence, and costs. Infect Dis Clin North Am. 2003, 17 (2), 227–
241. doi: 10.1016/S0891-5520(03)00005-9. https://www.ncbi.nlm.nih.
gov/pubmed/12601337
Foxman B., Somsel P., Tallman P., Gillespie B., Raz R., Colodner R. i wsp.: Urinary
tract infection among women aged 40 to 65: behavioral and sexual risk
factors. J Clin Epidemiol. 2001, 54 (7), 710–718. doi: 10.1016/s0895-
4356(00)00352-8. https://www.ncbi.nlm.nih.gov/pubmed/11438412
Fulop T.: Acute Pyelonephritis Workup. 2012. (updated: Dec 2018). http://
emedicine.medscape.com/article/245559-workup
Furr J., Watts T., Street R., Cross B., Slobodov G., Patel S.: Contemporary Trends
in the Inpatient Management of Fournier’s Gangrene: Predictors of Length
of Stay and Mortality Based on Population-based Sample. Urology. 2017,
102, 79–84. doi: 10.1016/j.urology.2016.09.021. https://www.ncbi.nlm.
nih.gov/pubmed/27693572
Garcia-Perdomo H.A., López H., Carbonell J., Castillo D., Cataño J.G., Serón P.:
Efficacy of antibiotic prophylaxis in patients undergoing cystoscopy: A randomized clinical trial. World J Urol. 2013, 31 (6), 1433–1439. doi: 10.1007/
s00345-013-1034-2. https://www.ncbi.nlm.nih.gov/pubmed/23412704
Garibaldi R.A., Burke J.P., Dickman M.L., Smith C.B.: Factors predisposing
to bacteriuria during indwelling urethral catheterization. N Engl J Med.
1974, 291 (5), 215–219. doi: 10.1056/NEJM197408012910501. https://
www.ncbi.nlm.nih.gov/pubmed/4834750
Geerlings S.E.: SWAB Guidelines for Antimicrobial Therapy of Complicated
Urinary Tract Infections in Adults. SWAB Guidelines, 2013. https://www.
ncbi.nlm.nih.gov/pubmed/17100128
Gerstner G.J., Müller G., Nahler G.: Amoxicillin in the treatment of asymptomatic bacteriuria in pregnancy: a single dose of 3 g amoxicillin versus a
4-day course of 3 doses 750 mg amoxicillin. Gynecol Obstet Invest. 1989,
27 (2), 84–87. doi: 10.1159/000293624. https://www.ncbi.nlm.nih.gov/
pubmed/2659442
Ghafoori M., Shakiba M., Seifmanesh H., Hoseini K.: Decrease in infection
rate following use of povidone-iodine during transrectal ultrasound guided
biopsy of the prostate: a double blind randomized clinical trial. Iranian J
Radiol. 2012, 9 (2), 67–70. doi: 10.5812/iranjradiol.7561. https://www.
ncbi.nlm.nih.gov/pubmed/23329966
Gill B.C., Shoskes D.A.: Bacterial prostatitis. Curr Opin Infect Dis. 2016, 29
(1), 86–91. doi: 10.1097/QCO.0000000000000222. https://www.ncbi.nlm.
nih.gov/pubmed/26555038
Gleckman R., Esposito A., Crowley M., Natsios G.A.: Reliability of a single
urine culture in establishing diagnosis of asymptomatic bacteriuria in adult
males. J Clin Microbiol. 1979, 9 (5), 596–597. https://www.ncbi.nlm.nih.
gov/pubmed/383746
Goff D.A., Kullar R., Goldstein E.J.C., Gilchrist M., Nathwani D., Cheng A.C.
i wsp.: A global call from five countries to collaborate in antibiotic stewardship: united we succeed, divided we might fail. Lancet Infect Dis. 2017, 17
(2), e56–e63. doi: 10.1016/S1473-3099(16)30386-3. https://www.ncbi.
nlm.nih.gov/pubmed/27866945
Gold E.M., Traub F.B., Daichman I., Terris M.: Asymptomatic bacteriuria during pregnancy. Obstet Gynecol. 1966, 27 (2), 206–209. https://www.ncbi.
nlm.nih.gov/pubmed/5325600
Gould C.V., Umscheid C.A., Agarwal R.K., Kuntz G., Pegues D.A.: Guideline
for prevention of catheter-associated urinary tract infections 2009. Infect
Control Hosp Epidemiol. 2010, 31 (4), 319–326. doi: 10.1086/651091. https://
www.ncbi.nlm.nih.gov/pubmed/20156062
Grabe M., Forsgren A., Björk T., Hellsten S.: Controlled trial of a short and a
prolonged course with ciprofloxacin in patients undergoing transurethral
prostatic surgery. Eur J Clin Microbiol. 1987, 6 (1), 11–17. doi.: 10.1007/
bf02097183. https://www.ncbi.nlm.nih.gov/pubmed/3569248
Grabe M., Forsgren A., Hellsten S.: The effect of a short antibiotic course
in transurethral prostatic resection. Scand J Urol Nephrol. 1984, 18 (1),
37–42. doi: 10.3109/00365598409182161. https://www.ncbi.nlm.nih.
gov/pubmed/6202000
Green H., Rahamimov R., Goldberg E., Leibovici L., Gafter U., Bishara J. i wsp.:
Consequences of treated versus untreated asymptomatic bacteriuria in the
first year following kidney transplantation: Retrospective observational
study. Eur J Clin Microbiol Infect Dis. 2013, 32 (1), 127–131. doi: 10.1007/
s10096-012-1727-2. https://www.ncbi.nlm.nih.gov/pubmed/22918514
Guenaga K.F., Matos D., Wille-Jørgensen P.: Mechanical bowel preparation for
elective colorectal surgery. Cochrane Database Syst Rev, 2011: CD001544.
doi: 10.1002/14651858.CD001544.pub4. https://www.ncbi.nlm.nih.gov/
pubmed/21901677
Gupta K., Hooton T.M., Naber K.G., Wullt B., Colgan R., Miller L.G. i wsp.:
International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious
Diseases Society of America and the European Society for Microbiology and
Infectious Diseases. Clin Infect Dis. 2011, 52 (2), e103. doi: 10.1093/cid/
ciq257. https://www.ncbi.nlm.nih.gov/pubmed/21292654
Gupta K., Hooton T.M., Roberts P.L., Stamm W.E.: Short-course nitrofurantoin
for the treatment of acute uncomplicated cystitis in women. Arch Intern
Med. 2007, 167, 2207–2212. doi: 10.1001/archinte.167.20.2207. https://
www.ncbi.nlm.nih.gov/pubmed/17998493
Gupta K., Stamm W.E.: Outcomes associated with trimethoprim/sulphamethoxazole (TMP/SMX) therapy in TMP/SMX resistant community-acquired
UTI. Int J Antimicrob Agents. 2002, 19 (6), 554–556. doi: 10.1016/s0924-
8579(02)00104-8. https://www.ncbi.nlm.nih.gov/pubmed/12135847
Gurbuz C., Güner B., Atış G., Canat L., Caşkurlu T.: Are prophylactic antibiotics necessary for urodynamic study? Kaohsiung J Med Sci. 2013, 29
(6), 325. doi: 10.1016/j.kjms.2012.06.001. https://www.ncbi.nlm.nih.gov/
pubmed/20377490
Guyatt G.H., Oxman A.D., Kunz R., Falck-Ytter Y., Vist G.E., Liberati A. i wsp.:
Going from evidence to recommendations. BMJ. 2008, 336, 1049–1051.
doi: 10.1136/bmj.39493.646875.AE. https://www.ncbi.nlm.nih.gov/
pubmed/18467413
Guyatt G.H., Oxman A.D., Kunz R., Vist G.E., Falck-Ytter Y., Schunemann H.J.:
What is “quality of evidence” and why is it important to clinicians? BMJ.
2008, 336, 995–998. doi: 10.1136/bmj.39490.551019.BE. https://www.
ncbi.nlm.nih.gov/pubmed/18456631
Haddadeen C., Dickinson L., Chawishly E., Lau R., Watkin N.: Comparative
regional audit of urology and genito-urinary departments in the management of acute epididymo-orchitis. HIV Medicine. 2010, 11, 45. https://
www.ncbi.nlm.nih.gov/pubmed/70186144
Haggerty C.L., Gottlieb S.L., Taylor B.D., Low N., Xu F., Ness R.B.: Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis.
2010, 201 Suppl 2, S134–S155. doi: 10.1086/652395. https://www.ncbi.
nlm.nih.gov/pubmed/20470050
Hansson S., Jodal U., Lincoln K., Svanborg-Edén C.: Untreated asymptomatic
bacteriuria in girls: II – Effect of phenoxymethylpenicillin and erythromycin given for intercurrent infections. BMJ. 1989, 298 (6677), 856–
859. doi: 10.1136/bmj.298.6677.856. https://www.ncbi.nlm.nih.gov/
pubmed/2497823
Hara R., Jo Y., Fujii T., Kondo N., Yokoyoma T., Miyaji Y.: Optimal approach for
prostate cancer detection as initial biopsy: prospective randomized study
comparing transperineal versus transrectal systematic 12-core biopsy.
Urology. 2008, 71 (2), 191–195. doi: 10.1016/j.urology.2007.09.029. https://
www.ncbi.nlm.nih.gov/pubmed/18308081
Harbarth S., Holeckova K., Froidevaux C., Pittet D., Ricou B., Grau G.E. i wsp.:
Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care
Med. 2001, 164 (3), 396–402. doi: 10.1164/ajrccm.164.3.2009052. https://
www.ncbi.nlm.nih.gov/pubmed/11500339
Harding G.K., Zhanel G.G., Nicolle L.E., Cheang M.: Antimicrobial treatment
in diabetic women with asymptomatic bacteriuria. N Engl J Med. 2002,
347 (20), 1576–1583. doi: 10.1056/NEJMoa021042. https://www.ncbi.
nlm.nih.gov/pubmed/12432044
Harnisch J.P., Berger R.E., Alexander E.R., Monda G., Holmes K.K.: Aetiology
of acute epididymitis. Lancet. 1977, 1, 819–821. doi: 10.1016/s0140-
6736(77)92773-8. https://www.ncbi.nlm.nih.gov/pubmed/67333
Harris R.E., Gilstrap L.C., Pretty A.: Single-dose antimicrobial therapy for
asymptomatic bacteriuria during pregnancy. Obstet Gynecol. 1982, 59 (5),
546–549. https://www.ncbi.nlm.nih.gov/pubmed/7070725
Hartstein A.I., Garber S.B., Ward T.T., Jones S.R., Morthland V.H.: Nosocomial
urinary tract infection: a prospective evaluation of 108 catheterized patients.
Infect Control. 1981, 2 (5), 380–386. doi: 10.1017/s0195941700055533.
https://www.ncbi.nlm.nih.gov/pubmed/6795141
Hermanides H.S., Hulscher M.E., Schouten J.A., Prins J.M., Geerlings S.E.:
Development of quality indicators for the antibiotic treatment of complicated urinary tract infections: a first step to measure and improve care. Clin
Infect Dis. 2008, 46 (5), 703–711. doi: 10.1086/527384. https://www.ncbi.
nlm.nih.gov/pubmed/18230045
Heyns C.F.: Urinary tract infection associated with conditions causing urinary tract obstruction and stasis, excluding urolithiasis and neuropathic
bladder. World J Urol. 2012, 30 (1), 77–83. doi: 10.1007/s00345-011-0725-
9. https://www.ncbi.nlm.nih.gov/pubmed/21720861
Hill J.B., Sheffield J.S., McIntire D.D., Wendel G.D. Jr.: Acute pyelonephritis in pregnancy. Obstet Gynecol. 2005, 105 (1), 18–23. doi: 10.1097/01.
AOG.0000149154.96285.a0. https://www.ncbi.nlm.nih.gov/pubmed/15625136
Hirakauva E., Bianchi-Ferraro A.M., Zucchi E.V.M., Kajikawa M.M., Girão M.J.,
Sartori M.G.: Incidence of urinary infection in women after urodynamic
study (UDS). Int Urogynecol J Pelvic Floor Dysfunct, 2011. 22.
Hooton T.M.: Clinical practice. Uncomplicated urinary tract infection. N
Engl J Med. 2012, 366 (11), 1028–1037. doi: 10.1056/NEJMcp1104429.
https://www.ncbi.nlm.nih.gov/pubmed/22417256
Hooton T.M.: Prevention of recurrent urogenital tract infections in adult
women, In: EAU/International Consultation on Urological Infections.
European Association of Urology: The Netherlands, 2010.
Hooton T.M.: Recurrent urinary tract infection in women. Int J Antimicrob
Agents. 2001, 17 (4), 259–268. doi: 10.1016/s0924-8579(00)00350-2. https://
www.ncbi.nlm.nih.gov/pubmed/11295405
Hooton T.M., Bradley S.F., Cardenas D.D., Colgan R., Geerlings S.E., Rice J.C.
i wsp.: Diagnosis, prevention, and treatment of catheter-associated urinary
tract infection in adults: 2009 International Clinical Practice Guidelines
from the Infectious Diseases Society of America. Clin Infect Dis. 2010,
50 (5), 625–663. doi: 10.1086/650482. https://www.ncbi.nlm.nih.gov/
pubmed/20175247
Hooton T.M., Roberts P.L., Stapleton A.E.: Cefpodoxime vs ciprofloxacin for
short-course treatment of acute uncomplicated cystitis: a randomized trial.
JAMA. 2012, 307 (6), 583–589. doi: 10.1001/jama.2012.80. https://www.
ncbi.nlm.nih.gov/pubmed/22318279
Hooton T.M., Scholes D., Gupta K., Stapleton A.E., Roberts P.L., Stamm W.E.:
Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated
cystitis in women: a randomized trial. Jama. 2005, 293 (8), 949–955. doi:
10.1001/jama.293.8.949. https://www.ncbi.nlm.nih.gov/pubmed/15728165
Horan T.C., Andrus M., Dudeck M.A.: CDC/NHSN surveillance definition
of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008, 36 (5) 309–
332. doi: 10.1016/j.ajic.2008.03.002. https://www.ncbi.nlm.nih.gov/
pubmed/18538699
Horner P.J., Blee K., Falk L., van der Meijden W., Moi H.: 2016 European guideline on the management of non-gonococcal urethritis. Int J STD AIDS.
2016, 27 (11), 928–937. doi: 10.1177/0956462416648585. https://www.
ncbi.nlm.nih.gov/pubmed/27147267
Hotchkiss, R.S., Karl I.E.: The pathophysiology and treatment of sepsis. N
Engl J Med. 2003, 348 (2), 138–150. doi: 10.1056/NEJMra021333. https://
www.ncbi.nlm.nih.gov/pubmed/12519925
Howell M.D., Davis A.M.: Management of Sepsis and Septic Shock. JAMA.
2017, 317 (8), 847–848. doi: 10.1001/jama.2017.0131. https://www.ncbi.
nlm.nih.gov/pubmed/28114603
Hsieh C.H., Yang S.S., Chang S.J.: The Effectiveness of Prophylactic Antibiotics
with Oral Levofloxacin against Post-Shock Wave Lithotripsy Infectious
Complications: A Randomized Controlled Trial. Surg Infect (Larchmit).
2016, 17 (3), 346–351. doi: 10.1089/sur.2015.129. https://www.ncbi.nlm.
nih.gov/pubmed/26910613
Hua L.X., Zhang J.X., Wu H.F., Zhang W., Qian L.X., Xia G.W. i wsp.: [The
diagnosis and treatment of acute prostatitis: report of 35 cases]. Zhonghua
Nan Ke Xue. 2005, 11 (12), 897–899. https://www.ncbi.nlm.nih.gov/
pubmed/16398358
Hulscher M.E., Grol R.P., van der Meer J.W.: Antibiotic prescribing in hospitals: a social and behavioural scientific approach. Lancet Infect Dis. 2010,
10 (3), 167–175. doi: 10.1016/S1473-3099(10)70027-X. https://www.ncbi.
nlm.nih.gov/pubmed/20185095
Huttner A., Verhaegh E.M., Harbarth S., Muller A.E., Theuretzbacher U., Mouton
J.W.: Nitrofurantoin revisited: a systematic review and meta-analysis of
controlled trials. J Antimicrob Chemother. 2015, 70 (9), 2456–2464. doi:
10.1093/jac/dkv147. https://www.ncbi.nlm.nih.gov/pubmed/26066581
Isen K., Küpeli B., Sinik Z., Sözen S., Bozkirli I.: Antibiotic prophylaxis for
transrectal biopsy of the prostate: A prospective randomized study
of the prophylactic use of single dose oral fluoroquinolone versus trimethoprim-sulfamethoxazole. Int Urol Nephrol. 1999, 31 (4), 491–
495. doi: 10.1023/a:1007115312039. https://www.ncbi.nlm.nih.gov/
pubmed/10668944
Ito S., Hanaoka N., Shimuta K., Seike K., Tsuchiya T., Yasuda M. i wsp.: Male nongonococcal urethritis: From microbiological etiologies to demographic and
clinical features. Int J Urol. 2016, 23 (4), 325–331. doi: 10.1111/iju.13044.
https://www.ncbi.nlm.nih.gov/pubmed/26845624
Jacobsen S.M., Stickler D.J., Mobley H.L., Shirtliff M.E.: Complicated catheterassociated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clin Microbiol Rev. 2008, 21 (1), 26–59. doi: 10.1128/CMR.00019-07.
https://www.ncbi.nlm.nih.gov/pubmed/18202436
Jallali N., Withey S., Butler P.E.: Hyperbaric oxygen as adjuvant therapy in
the management of necrotizing fasciitis. Am J Surg. 2005, 189 (4), 462–
466. doi: 10.1016/j.amjsurg.2005.01.012. https://www.ncbi.nlm.nih.gov/
pubmed/15820462
Jepson R.G., Williams G., Craig J.C.: Cranberries for preventing urinary
tract infections. Cochrane Database Syst Rev. 2012, 10, CD001321. doi:
10.1002/14651858.CD001321.pub5. https://www.ncbi.nlm.nih.gov/
pubmed/23076891
Jimenez-Cruz J.F., Tormo F.B., Gómez J.G.: Treatment of chronic prostatitis:
intraprostatic antibiotic injections under echography control. J Urol. 1988,
139 (5), 967–970. doi: 10.1016/s0022-5347(17)42733-9. https://www.ncbi.
nlm.nih.gov/pubmed/3283385
Johansen T.E., Botto H., Cek M., Grabe M., Tenke P., Wagenlehner F.M. i wsp.:
Critical review of current definitions of urinary tract infections and proposal
of an EAU/ESIU classification system. Int J Antimicrob Agents. 2011, 38
Suppl. 64–70. doi: 10.1016/j.ijantimicag.2011.09.009. https://www.ncbi.
nlm.nih.gov/pubmed/22018988
Kanjanawongdeengam P., Viseshsindh W., Santanirand P., Prathombutr P.,
Nilkulwattana S.: Reduction in bacteremia rates after rectum sterilization
before transrectal, ultrasound-guided prostate biopsy: a randomized controlled trial. J Med Assoc Thai. 2009, 92 (12), 1621–1626. https://www.
ncbi.nlm.nih.gov/pubmed/20043564
Kapoor D.A., Klimberg I.W., Malek G.H., Wegenke J.D., Cox C.E., Patterson A.L.
i wsp.: Single-dose oral ciprofloxacin versus placebo for prophylaxis during
transrectal prostate biopsy. Urology. 1998, 52 (4), 552–558. doi: 10.1016/
s0090-4295(98)00296-9. https://www.ncbi.nlm.nih.gov/pubmed/9763070
Karian L.S., Chung S.Y., Lee E.S.: Reconstruction of Defects After Fournier
Gangrene: A Systematic Review. Eplasty. 2015, 15, e18. https://www.ncbi.
nlm.nih.gov/pubmed/26171090
Kass E.H.: Asymptomatic infections of the urinary tract. Trans Assoc
Am Physicians. 1956, 69, 56–64. https://www.ncbi.nlm.nih.gov/
pubmed/13380946
Kass E.H.: Pyelonephritis and bacteriuria. A major problem in preventive
medicine. Ann Intern Med. 1962, 56, 46–53. doi: 10.7326/0003-4819-56-
1-46. https://www.ncbi.nlm.nih.gov/pubmed/14454174
Kazemier B.M., Koningstein F.N., Schneeberger C., Ott A., Bossuyt P.M., de
Miranda E. i wsp.: Maternal and neonatal consequences of treated and
untreated asymptomatic bacteriuria in pregnancy: a prospective cohort
study with an embedded randomised controlled trial. Lancet Infect Dis.
2015, 15 (11), 1324–1333. doi: 10.1016/S1473-3099(15)00070-5. https://
www.ncbi.nlm.nih.gov/pubmed/26255208
Kim S.Y., Dupree J.M., Le B.V., Kim D.Y., Zhao L.C., Kundu S.D.: A Contemporary
Analysis of Fournier Gangrene Using the National Surgical Quality
Improvement Program. Urology. 2015, (5), 1052–1057. doi: 10.1016/j.
urology.2014.08.063. https://www.ncbi.nlm.nih.gov/pubmed/25770725
Kincaid-Smith P., Bullen M.: Bacteriuria in Pregnancy. Lancet. 1965, 1, 395–
399. doi: 10.1016/s0140-6736(65)90001-2. https://www.ncbi.nlm.nih.
gov/pubmed/14238090
Kirkcaldy R.D., Harvey A., Papp J.R., Del Rio C., Soge O.O., Holmes K.K. i wsp.:
Neisseria gonorrhoeae Antimicrobial Susceptibility Surveillance - The
Gonococcal Isolate Surveillance Project, 27 Sites, United States, 2014. MMWR
Surveill Summ. 2016, 65 (7), 1–19. doi: 10.15585/mmwr.ss6507a1. https://
www.ncbi.nlm.nih.gov/pubmed/27414503
Kontiokari T., Sundqvist K., Nuutinen M., Pokka T., Koskela M., Uhari M.:
Randomised trial of cranberry-lingonberry juice and Lactobacillus GG drink
for the prevention of urinary tract infections in women. BMJ. 2001, 322,
1571. doi: 10.1136/bmj.322.7302.1571. https://www.ncbi.nlm.nih.gov/
pubmed/11431298
Koves B., Cai T., Veeratterapillay R., Pickard R., Seisen T., Lam T.B. i wsp.: Benefits
and Harms of Treatment of Asymptomatic Bacteriuria: A Systematic Review
and Meta-analysis by the European Association of Urology Urological
Infection Guidelines Panel. Eur Urol. 2017, 72 (6), 865–868. doi: 10.1016/j.
eururo.2017.07.014. https://www.ncbi.nlm.nih.gov/pubmed/28754533
Kranjcec B., Papes D., Altarac S.: D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J
Urol. 2014, 32 (1), 79–84. doi: 10.1007/s00345-013-1091-6. https://www.
ncbi.nlm.nih.gov/pubmed/23633128
Krieger J.N.: Recurrent lower urinary tract infections in men. J New Rem
Clin. 1998, 47, 4.
Krieger J.N.: Trichomoniasis in men: old issues and new data. Sex Transm
Dis. 1995, 22 (2), 83–96. https://www.ncbi.nlm.nih.gov/pubmed/7624817
Krieger J.N., Egan K.J., Ross S.O., Jacobs R., Berger R.E.: Chronic pelvic pains
represent the most prominent urogenital symptoms of “chronic prostatitis”. Urology. 1996, 48 (5), 715–721. doi: 10.1016/S0090-4295(96)00421-9.
https://www.ncbi.nlm.nih.gov/pubmed/8911515
Krieger J.N., Nyberg L. Jr, Nickel J.C.: NIH consensus definition and classification of prostatitis. JAMA. 1999, 282 (3), 236–237. doi: 10.1001/
jama.282.3.236. https://www.ncbi.nlm.nih.gov/pubmed/10422990
Kunin C.M., McCormack R.C.: Prevention of catheter-induced urinary-tract
infections by sterile closed drainage. N Engl J Med. 1966, 274 (21), 1155–
1161. doi: 10.1056/NEJM196605262742101. https://www.ncbi.nlm.nih.
gov/pubmed/5934951
Kunin C.M.: Urinary tract infections: detection, prevention and management. 5th ed. Williams and Wilkins, Baltimore 1997.
Lauerman M., Kolesnik O., Sethuraman K., Rabinowitz R., Joshi M., Clark E.
i wsp.: Less is More? Antibiotic duration and outcomes in fournier’s gangrene. J Trauma Acute Care Surg. 2017, 83 (3), 443–448. doi: 10.1097/
TA.0000000000001562. https://www.ncbi.nlm.nih.gov/pubmed/28538648
Lecomte F., Allaert F.A.: Single-dose treatment of cystitis with fosfomycin
trometamol (Monuril): analysis of 15 comparative trials on 2,048 patients.
Giorn It Ost Gin. 1997, 19, 399.
Levy M.M., Fink M.P., Marshall J.C., Abraham E., Angus D., Cook D. i wsp.:
2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions
Conference. Crit Care Med. 2003, 31 (4), 1250–1256. doi: 10.1097/01.
CCM.0000050454.01978.3B. https://www.ncbi.nlm.nih.gov/
pubmed/12682500
Li C., Zhou X., Liu L.F., Qi F., Chen J.B., Zu X.B.: Hyperbaric oxygen therapy as
an adjuvant therapy for comprehensive treatment of Fournier’s gangrene.
Urol Int. 2015, 94 (4), 453–458. doi: 10.1159/000366137. https://www.
ncbi.nlm.nih.gov/pubmed/25677386
Lifshitz E., Kramer L.: Outpatient urine culture: does collection technique
matter? Arch Intern Med. 2000, 160 (16), 2537–2540. doi: 10.1001/
archinte.160.16.2537. https://www.ncbi.nlm.nih.gov/pubmed/10979067
Liker Y., Türkeri L., Korten V., Tarvan T., Özveri H., Simsek F.: The role of antibiotics in patients with increased risk of infection during extracorporeal
shock wave lithotripsy (ESWL) treatment. Marmara Med J. 1996, 9, 174–
177. https://www.ncbi.nlm.nih.gov/pubmed/26377368
Lindert K.A., Kabalin J.N., Terris M.K.: Bacteremia and bacteriuria after transrectal ultrasound guided prostate biopsy. J Urol. 2000, 164 (1), 76–80.
https://www.ncbi.nlm.nih.gov/pubmed/10840428
Lipsky B.A., Byren I., Hoey C.T.: Treatment of bacterial prostatitis. Clin Infect
Dis. 2010, 50, 1641–1652. doi: 10.1086/652861. https://www.ncbi.nlm.
nih.gov/pubmed/20459324
Lista F., Redondo C., Meilán E., García-Tello A., Ramón de Fata F., Angulo J.C.:
Efficacy and safety of fosfomycin-trometamol in the prophylaxis for transrectal prostate biopsy. Prospective randomized comparison with ciprofloxacin.
Actas Urol Esp. 2014, 38 (6), 391–396. doi: 10.1016/j.acuro.2014.01.002.
https://www.ncbi.nlm.nih.gov/pubmed/24775812
Little P.J.: The incidence of urinary infection in 5000 pregnant women.
Lancet. 1966, 2, 925–928. doi: 10.1016/s0140-6736(66)90534-4. https://
www.ncbi.nlm.nih.gov/pubmed/4162367
Litwin M.S., McNaughton-Collins M., Fowler F.J. Jr, Nickel J.C., Calhoun E.A.,
Pontari M.A. i wsp.: The National Institutes of Health chronic prostatitis
symptom index: development and validation of a new outcome measure.
Chronic Prostatitis Collaborative Research Network. J Urol. 1999, 162 (2),
369–375. doi: 10.1016/s0022-5347(05)68562-x. https://www.ncbi.nlm.
nih.gov/pubmed/10411041
Lo C.W., Yang S.S., Hsieh C.H., Chang S.J.: Effectiveness of Prophylactic
Antibiotics against Post-Ureteroscopic Lithotripsy Infections: Systematic
Review and Meta-Analysis. Surg Infect. 2015, 16 (4), 415–420. doi: 10.1089/
sur.2014.013. https://www.ncbi.nlm.nih.gov/pubmed/26207401
Ludwig M., Schroeder-Printzen I., Schiefer H.G., Weidner W.: Diagnosis and
therapeutic management of 18 patients with prostatic abscess. Urology.
1999, 53 (2), 340–345. doi: 10.1016/s0090-4295(98)00503-2. https://www.
ncbi.nlm.nih.gov/pubmed/9933051
Lumbiganon P., Villar J., Laopaiboon M., Widmer M., Thinkhamrop J., Carroli
G. i wsp.: One-day compared with 7-day nitrofurantoin for asymptomatic
bacteriuria in pregnancy: A randomized controlled trial. Obstet Gynecol.
2009, 113, 339–345. doi: 10.1097/AOG.0b013e318195c2a2. https://www.
ncbi.nlm.nih.gov/pubmed/19155904
Lutay N., Ambite I., Grönberg Hernandez J., Rydström G., Ragnarsdóttir B., Puthia
M. i wsp.: Bacterial control of host gene expression through RNA polymerase II. J Clin Invest. 2013, 123 (6), 2366–2379. doi: 10.1172/JCI66451.
https://www.ncbi.nlm.nih.gov/pubmed/23728172
Lu Y., Tianyong F., Ping H., Liangren L., Haichao Y., Qiang W.: Antibiotic prophylaxis for shock wave lithotripsy in patients with sterile urine before treatment may be unnecessary: A systematic review and meta-analysis. J Urol.
2012, 188 (2), 441–448. doi: 10.1016/j.juro.2012.04.014. https://www.
ncbi.nlm.nih.gov/pubmed/22704118
Madersbacher H., van Ophoven A., van Kerrebroeck P.E.: GAG layer replenishment therapy for chronic forms of cystitis with intravesical glycosaminoglycans – a review. Neurourol Urodyn. 2013, 32 (1), 9–18. doi: 10.1002/
nau.22256. https://www.ncbi.nlm.nih.gov/pubmed/22782909
Maki D.G., Tambyah P.A.: Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001, 7 (2), 342–347. doi: 10.3201/
eid0702.010240. https://www.ncbi.nlm.nih.gov/pubmed/11294737
Marschall J., Carpenter C.R., Fowler S., Trautner B.W.: Antibiotic prophylaxis
for urinary tract infections after removal of urinary catheter: Meta-analysis.
BMJ. 2013, 346: f3147. doi: 10.1136/bmj.f3147. https://www.ncbi.nlm.
nih.gov/pubmed/23757735
Martin G.S., Mannino D.M., Eaton S., Moss M.: The epidemiology of sepsis
in the United States from 1979 through 2000. N Engl J Med. 2003, 348
(16), 1546–1554. doi: 10.1056/NEJMoa022139. https://www.ncbi.nlm.
nih.gov/pubmed/12700374
Masterton R.G., Evans D.C., Strike P.W.: Single-dose amoxycillin in the treatment of bacteriuria in pregnancy and the puerperium – a controlled clinical
trial. Br J Obstet Gynaecol. 1985, 92 (5), 498–505. doi: 10.1111/j.1471-
0528.1985.tb01355.x. https://www.ncbi.nlm.nih.gov/pubmed/3888250
Mayersak J.S.: Transrectal ultrasonography directed intraprostatic injection
of gentamycin-xylocaine in the management of the benign painful prostate syndrome. A report of a 5 year clinical study of 75 patients. Int Surg. 1998,
83, 347–349. https://www.ncbi.nlm.nih.gov/pubmed/10096759
Meares E.M., Stamey T.A.: Bacteriologic localization patterns in bacterial
prostatitis and urethritis. Invest Urol. 1968, 5 (5), 492–518. https://www.
ncbi.nlm.nih.gov/pubmed/4870505
Melekos M.D.: Efficacy of prophylactic antimicrobial regimens in preventing
infectious complications after transrectal biopsy of the prostate. Int Urol
Nephrol. 1990, 22 (3), 257–262. doi: 10.1007/bf02550403. https://www.
ncbi.nlm.nih.gov/pubmed/2210982
Meyer W.H., Huland H., Becker H.: Transrectal prostatic biopsy: The incidence of fever and sepsis after treatment with antibiotics. Aktuelle Urol,
1987. 18: 22.
Mikkelsen M.E., Miltiades A.N., Gaieski D.F., Goyal M., Fuchs B.D., Shah C.V.
i wsp.: Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009, 37 (5), 1670–
1677. doi: 10.1097/CCM.0b013e31819fcf68. https://www.ncbi.nlm.nih.
gov/pubmed/19325467
Millar L.K., Wing D.A., Paul R.H., Grimes D.A.: Outpatient treatment of pyelonephritis in pregnancy: a randomized controlled trial. Obstet Gynecol.
1995, 86, 560–564. doi: 10.1016/0029-7844(95)00244-l. https://www.
ncbi.nlm.nih.gov/pubmed/7675380
Mody L., Juthani-Mehta M.: Urinary tract infections in older women: a clinical review. JAMA. 2014, 311 (8), 844–854. doi: 10.1001/jama.2014.303.
https://www.ncbi.nlm.nih.gov/pubmed/24570248
Mombelli G., Pezzoli R., Pinoja-Lutz G., Monotti R., Marone C., Franciolli M.:
Oral vs intravenous ciprofloxacin in the initial empirical management of
severe pyelonephritis or complicated urinary tract infections: a prospective randomized clinical trial. Arch Intern Med. 1999, 159 (1), 53–58. doi:
10.1001/archinte.159.1.53. https://www.ncbi.nlm.nih.gov/pubmed/9892331
Monnet X., Marik P.E., Teboul J.L.: Prediction of fluid responsiveness: an
update. Ann Intensive Care. 2016, 6 (1), 111. doi: 10.1186/s13613-016-
0216-7. https://www.ncbi.nlm.nih.gov/pubmed/27858374
Moradi M., Abbasi M., Moradi A., Boskabadi A., Jalali A.: Effect of antibiotic
therapy on asymptomatic bacteriuria in kidney transplant recipients. Urol
J. 2005, 2 (1), 32–35. https://www.ncbi.nlm.nih.gov/pubmed/17629893
Mouncey P.R., Osborn T.M., Power G.S., Harrison D.A., Sadique M.Z., Grieve
R.D. i wsp.: Trial of early, goal-directed resuscitation for septic shock. N
Engl J Med. 2015, 372 (14), 1301–1311. doi: 10.1056/NEJMoa1500896.
https://www.ncbi.nlm.nih.gov/pubmed/25776532
Mrkobrada M., Ying I., Mokrycke S., Dresser G., Elsayed S., Bathini V. i wsp.:
CUA Guidelines on antibiotic prophylaxis for urologic procedures. Can Urol
Assoc J. 2015, 9, 13–22. doi: 10.5489/cuaj.2382. https://www.ncbi.nlm.
nih.gov/pubmed/25737749
Mulla N.: Bacteriuria in pregnancy. Obstet Gynecol. 1960, 16, 89–92. https://
www.ncbi.nlm.nih.gov/pubmed/14425118
Murphy D.M., Stassen L., Carr M.E., Gillespie W.A., Cafferkey M.T., Falkiner
F.R.: Bacteraemia during prostatectomy and other transurethral operations:
influence of timing of antibiotic administration. J Clin Pathol. 1984, 37
(6), 673–676. doi: 10.1136/jcp.37.6.673. https://www.ncbi.nlm.nih.gov/
pubmed/6725613
Naber K.G., Cho Y.H., Matsumoto T., Schaeffer A.J.: Immunoactive prophylaxis of recurrent urinary tract infections: a meta-analysis. Int J Antimicrob
Agents. 2009, 33 (2), 111–119. doi: 10.1016/j.ijantimicag.2008.08.011.
https://www.ncbi.nlm.nih.gov/pubmed/18963856
Naber K.G., Pilatz A., Weidner W., Naber K.: Prostatitits, epididymitis and orchitis. W: Red. D. Armstrong, J. Cohen, Infectious diseases. Mosby, London 1999.
Naber K.G., Schito G., Botto H., Palou J., Mazzei T.: Surveillance study in Europe
and Brazil on clinical aspects and Antimicrobial Resistance Epidemiology in
Females with Cystitis (ARESC): implications for empiric therapy. Eur Urol.
2008, 54 (5), 1164–1175. doi: 10.1016/j.eururo.2008.05.010. https://www.
ncbi.nlm.nih.gov/pubmed/18511178
Nicholson A., Rait G., Murray-Thomas T., Hughes G., Mercer C.H., Cassell J.:
Management of epididymo-orchitis in primary care: Results from a large UK
primary care database. Br J Gen Pract. 2010, 60, e407–422. doi: 10.3399/
bjgp10X532413. https://www.ncbi.nlm.nih.gov/pubmed/20883615
Nickel J.C.: Effective office management of chronic prostatitis. Urol Clin
North Am. 1998, 25 (4), 677–684. doi: 10.1016/s0094-0143(05)70056-2.
https://www.ncbi.nlm.nih.gov/pubmed/10026774
Nickel J.C., Shoskes D., Wang Y., Alexander R.B., Fowler J.E. Jr, Zeitlin S. i wsp.:
How does the pre-massage and post-massage 2-glass test compare to the
Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006, 176 (1), 119–124. doi: 10.1016/S0022-
5347(06)00498-8. https://www.ncbi.nlm.nih.gov/pubmed/16753385
Nicolle L.E.: Asymptomatic bacteriuria in the elderly. Infect Dis Clin North
Am. 1997, 11 (3), 647–662. doi: 10.1016/s0891-5520(05)70378-0. https://
www.ncbi.nlm.nih.gov/pubmed/9378928
Nicolle L.E.: Pivmecillinam in the treatment of urinary tract infections. J
Antimicrob Chemother. 2000, 46 Suppl 1, 35–39. https://www.ncbi.nlm.
nih.gov/pubmed/11051622
Nicolle L.E.: Urinary tract infections in patients with spinal injuries. Curr
Infect Dis Rep. 2014, 16 (1), 390. doi: 10.1007/s11908-013-0390-9. https://
www.ncbi.nlm.nih.gov/pubmed/24445675
Nicolle L.E., Bjornson J., Harding G.K., MacDonell J.A.: Bacteriuria in elderly
institutionalized men. N Engl J Med. 1983, 309 (23), 1420–1425. doi:
10.1056/NEJM198312083092304. https://www.ncbi.nlm.nih.gov/
pubmed/6633618
Nicolle L.E., Bradley S., Colgan R., Rice J.C., Schaeffer A., Hooton T.M.: Infectious
diseases society of America guidelines for the diagnosis and treatment of
asymptomatic bacteriuria in adults. Clin Infect Dis. 2005, 40 (5), 643–654.
doi: 10.1086/427507.https://www.ncbi.nlm.nih.gov/pubmed/15714408
Nicolle L.E., Mayhew W.J., Bryan L.: Prospective randomized comparison
of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987, 83 (1), 27–33. doi: 10.1016/0002-
9343(87)90493-1. https://www.ncbi.nlm.nih.gov/pubmed/3300325
Ohkawa M., Yamaguchi K., Tokunaga S., Nakashima T., Shoda R.: Antimicrobial
treatment for chronic prostatitis as a means of defining the role of Ureaplasma
urealyticum. Urol Int. 1993, 51 (3), 129–132. doi: 10.1159/000282530.
https://www.ncbi.nlm.nih.gov/pubmed/8249222
Olsen L., Nielsen I.K., Zachariassen A., Sederberg-Olsen J., Frimodt-Möller N.:
Single-dose versus six-day therapy with sulfamethizole for asymptomatic
bacteriuria during pregnancy. A prospective randomised study. Dan Med Bull.
1989, 36 (5), 486–487. https://www.ncbi.nlm.nih.gov/pubmed/2680315
Origuen J., López-Medrano F., Fernández-Ruiz M., Polanco N., Gutiérrez E.,
González E. i wsp.: Should asymptomatic bacteriuria be systematically treated
in kidney transplant recipients? Results from a randomized controlled trial.
Am J Transplant. 2016, 16 (10), 2943–2953. doi: 10.1111/ajt.13829. https://
www.ncbi.nlm.nih.gov/pubmed/27088545
Ouslander J.G., Schapira M., Schnelle J.F., Uman G., Fingold S., Tuico E.L.: Does
eradicating bacteriuria affect the severity of chronic urinary incontinence
in nursing home residents? Ann Intern Med. 1995, 122 (10), 749–754. doi:
10.7326/0003-4819-122-10-199505150-00003. https://www.ncbi.nlm.
nih.gov/pubmed/7717597
Papp J.R., Schachter J., Gaydos C.A., Van Der Pol B.: Recommendations for
the Laboratory-Based Detection of Chlamydia trachomatis and Neisseria
gonorrhoeae — 2014. MMWR Recomm Rep. 2014, 63, 1–19. https://www.
ncbi.nlm.nih.gov/pubmed/24622331
Pathak U.N., Tang K., Williams L.L., Stuart K.L.: Bacteriuria of pregnancy:
results of treatment. J Infect Dis. 1969, 120, 91–103. doi: 10.1093/
infdis/120.1.91. https://www.ncbi.nlm.nih.gov/pubmed/5816817
Pedler S.J., Bint A.J.: Comparative study of amoxicillin-clavulanic acid and
cephalexin in the treatment of bacteriuria during pregnancy. Antimicrob
Agents Chemother. 1985, 27 (4), 508–510. doi: 10.1128/aac.27.4.508. https://
www.ncbi.nlm.nih.gov/pubmed/4004191
Perletti G., Marras E., Wagenlehner F.M., Magri V.: Antimicrobial therapy for
chronic bacterial prostatitis. Cochrane Database Syst Rev. 2013: CD009071.
doi: 10.1002/14651858.CD009071.pub2. https://www.ncbi.nlm.nih.gov/
pubmed/23934982
Peterson J., Kaul S., Khashab M., Fisher A., Kahn J.B.: Identification and pretherapy susceptibility of pathogens in patients with complicated urinary
tract infection or acute pyelonephritis enrolled in a clinical study in the
United States from November 2004 through April 2006. Clin Ther. 2007,
29 (10), 2215–2221. doi: 10.1016/j.clinthera.2007.10.008. https://www.
ncbi.nlm.nih.gov/pubmed/18042477
Pfau A., Sacks T.G.: Effective prophylaxis for recurrent urinary tract infections during pregnancy. Clin Infect Dis. 1992, 14 (4), 810–814. https://
www.ncbi.nlm.nih.gov/pubmed/1576275
Phillips B., Ball C., Sackett D., Badenoch D., Straus S., Haynes B. i wsp.:
Oxford Centre for Evidence-based Medicine Levels of Evidence.
Updated by Jeremy Howick March 2009. 1998. http://www.cebm.net/
oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
Pilatz A., Hossain H., Kaiser R., Mankertz A., Schüttler C.G., Domann E. i wsp.:
Acute Epididymitis Revisited: Impact of Molecular Diagnostics on Etiology
and Contemporary Guideline Recommendations. Eur Urol. 2015, 68 (3),
428–435. doi: 10.1016/j.eururo.2014.12.005. https://www.ncbi.nlm.nih.
gov/pubmed/25542628
Pilatz A., Wagenlehner F., Hans-Christian S., Rusz A., Weidner W.: Impact of
bacterial epididymitis on semen quality after antibiotic treatment. J Urol.
2012, 1: e443. doi: 10.1016/j.juro.2012.02.1199. https://www.ncbi.nlm.
nih.gov/pubmed/70720788
Pitout J.D.: Infections with extended-spectrum beta-lactamase-producing
enterobacteriaceae: changing epidemiology and drug treatment choices.
Drugs. 2010, 70 (3), 313–333. doi: 10.2165/11533040-000000000-00000.
https://www.ncbi.nlm.nih.gov/pubmed/20166768
Plettenberg A.: STI – Sexually transmitted infections (Article in German).
Ifi-Card, 2nd Edition June 2014.
Polascik T.J., Oesterling J.E., Partin A.W.: Prostate specific antigen: a decade
of discovery – what we have learned and where we are going. J Urol. 1999,
162 (2), 293–306. doi: 10.1016/s0022-5347(05)68543-6. https://www.
ncbi.nlm.nih.gov/pubmed/10411025
Potts L., Cross S., MacLennan W.J., Watt B.: A double-blind comparative
study of norfloxacin versus placebo in hospitalised elderly patients with
asymptomatic bacteriuria. Arch Gerontol Geriatr. 1996, 23 (2), 153–161.
doi: 10.1016/0167-4943(96)00715-7. https://www.ncbi.nlm.nih.gov/
pubmed/15374159
Pregazzi R., Mazzatenta E., Bouchè C.: [Single-dose antibiotic therapy of asymptomatic bacteriuria in pregnancy. Results and complications]. Minerva Ginecol.
1987, 39 (4), 289–292. https://www.ncbi.nlm.nih.gov/pubmed/3601207
ProCESS Investigators, Yealy D.M., Kellum J.A., Huang D.T., Barnato A.E.,
Weissfeld L.A., Pike F. i wsp.: A randomized trial of protocol-based care for
early septic shock. N Engl J Med. 2014, 370 (18), 1683–1693. doi: 10.1056/
NEJMoa1401602. https://www.ncbi.nlm.nih.gov/pubmed/24635773
Radmayr C., Bogaert G., Dogan H.S., Kočvara R., Nijman J.M., Stein R. i wsp.:
EAU Guidelines on Paediatric Urology. In: EAU Guidelines, edition presented at the annual EAU Congress Barcelona 2019. ISBN 978-94-92671-
04-2. https://uroweb.org/guideline/paediatric-urology/
Raz R., Stamm W.E.: A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993,
329 (11), 753–756. doi: 10.1056/NEJM199309093291102. https://www.
ncbi.nlm.nih.gov/pubmed/8350884
Reeves D.S.: Laboratory and clinical studies with sulfametopyrazine as a
treatment for bacteriuria in pregnancy. J Antimicrob Chemother. 1975,
1 (2), 171–186. doi: 10.1093/jac/1.2.171. https://www.ncbi.nlm.nih.gov/
pubmed/1100589
Renneberg J., Paerregaard A.: Single-day treatment with trimethoprim for
asymptomatic bacteriuria in the elderly patient. J Urol, 1984, 132 (5), 934–
935. doi: 10.1016/s0022-5347(17)49954-x. https://www.ncbi.nlm.nih.gov/
pubmed/6387184
Reyner K., Heffner A.C., Karvetski C.H.: Urinary obstruction is an important
complicating factor in patients with septic shock due to urinary infection.
Am J Emerg Med. 2016, 34 (4), 694–696. doi: 10.1016/j.ajem.2015.12.068.
https://www.ncbi.nlm.nih.gov/pubmed/26905806
Riedl C.R., Plas E., Hübner W.A., Zimmerl H., Ulrich W., Pflüger H.: Bacterial
colonization of ureteral stents. Eur Urol. 1999, 36 (1), 53–59. doi:
10.1159/000019927. https://www.ncbi.nlm.nih.gov/pubmed/10364656
Rivers E., Nguyen B., Havstad S., Ressler J., Muzzin A., Knoblich B. i wsp.: Early
goal-directed therapy in the treatment of severe sepsis and septic shock.
N Engl J Med. 2001, 345 (19), 1368–1377. doi: 10.1056/NEJMoa010307.
https://www.ncbi.nlm.nih.gov/pubmed/11794169
Robertson J.G., Livingstone J.R., Isdale M.H.: The managment and complications of asymptomatic bacteriuria in pregnancy. Report of a study on
8,275 patients. J Obstet Gynaecol Br Commonw. 1968, 75 (1), 59–65. doi:
10.1111/j.1471-0528.1968.tb00121.x. https://www.ncbi.nlm.nih.gov/
pubmed/5635245
Robinson A.J., Grant J.B., Spencer R.C., Potter C., Kinghorn G.R.: Acute
epididymitis: why patient and consort must be investigated. Br J Urol. 1990,
66 (6), 642–645. doi: 10.1111/j.1464-410x.1990.tb07200.x. https://www.
ncbi.nlm.nih.gov/pubmed/2265337
Roghmann F., von Bodman C., Löppenberg B., Hinkel A., Palisaar J., Noldus J.:
Is there a need for the Fournier’s gangrene severity index? Comparison of
scoring systems for outcome prediction in patients with Fournier’s gangrene.
BJU Int. 2012, 110 (9), 1359–1365. doi: 10.1111/j.1464-410X.2012.11082.x.
https://www.ncbi.nlm.nih.gov/pubmed/22494217
Rosser C.J., Bare R.L., Meredith J.W.: Urinary tract infections in the critically ill patient with a urinary catheter. Am J Surg. 1999, 177 (4), 287–
290. doi: 10.1016/s0002-9610(99)00048-3. https://www.ncbi.nlm.nih.
gov/pubmed/10326844
Rubin R.H., Shapiro E.D., Andriole V.T., Davis R.J., Stamm W.E.: Evaluation
of new anti-infective drugs for the treatment of urinary tract infection. Infectious Clin Infect Dis. 1992, 15 Suppl 1, S216–S227. doi:
10.1093/clind/15.supplement_1.s216. https://www.ncbi.nlm.nih.gov/
pubmed/1477233
Rubin R.H., Shapiro E.D., Andriole V.T., Davis R.J., Stamm W.E.: General guidelines for the evaluation of new anti-infective drugs for the treatment of urinary tract infection. Eur J Clin Microbiol Infect Dis. Taukirchen, Germany.
1993, 240. doi: 10.1093/clind/15.supplement_1.s216. https://academic.
oup.com/cid/article/15/Supplement_1/S216/272999
Rudenko N., Dorofeyev A.: Prevention of recurrent lower urinary tract infections by long-term administration of fosfomycin trometamol. Double blind,
randomized, parallel group, placebo controlled study. Arzneimittelforschung.
2005, 55 (7), 420–427. doi: 10.1055/s-0031-1296881. https://www.ncbi.
nlm.nih.gov/pubmed/16080282
Ruebush I.T.K., McConville J.H., Calia F.M.: A double-blind study of trimethoprim-sulfamethoxazole prophylaxis in patients having transrectal needle biopsy of the prostate. J Urol. 1979, 122 (4), 492–494. doi: 10.1016/
s0022-5347(17)56477-0. https://www.ncbi.nlm.nih.gov/pubmed/384025
Saint S., Greene M.T., Fakih M.G.: Preventing Catheter-Associated Urinary
Tract Infections. N Engl J Med. 2016, 375 (13), 1298–1299. doi: 10.1056/
NEJMc1609988. https://www.ncbi.nlm.nih.gov/pubmed/27682041
Saint S., Lipsky B.A.: Preventing catheter-related bacteriuria: should we?
Can we? How? Arch Intern Med. 1999, 159 (8), 800–808. doi: 10.1001/
archinte.159.8.800. https://www.ncbi.nlm.nih.gov/pubmed/10219925
Schaeffer A.J.: Prostatitis: US perspective. Int J Antimicrob Agents. 1999,
11, 205–211. doi: 10.1016/s0924-8579(99)00046-1. https://www.ncbi.
nlm.nih.gov/pubmed/10394972
Schaeffer A.J., Datta N.S., Fowler J.E. Jr, Krieger J.N., Litwin M.S., Nadler
R.B i wsp.: Summary consensus statement: diagnosis and management
of chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2003, 43,
1–4. doi: 10.1016/s0090-4295(02)01979-9. https://www.ncbi.nlm.nih.
gov/pubmed/12521576
Schaeffer A.J., Stuppy B.A.: Efficacy and safety of self-start therapy in women
with recurrent urinary tract infections. J Urol. 1999, 161 (1), 207–211.
https://www.ncbi.nlm.nih.gov/pubmed/10037399
Schaeffer A.J., Wu S.C., Tennenberg A.M., Kahn J.B.: Treatment of chronic
bacterial prostatitis with levofloxacin and ciprofloxacin lowers serum
prostate specific antigen. J Urol. 2005, 174 (1), 161–164. doi: 10.1097/01.
ju.0000162017.24965.2b. https://www.ncbi.nlm.nih.gov/pubmed/15947609
Schneider H., Ludwig M., Hossain H.M., Diemer T., Weidner W.: The 2001
Giessen Cohort Study on patients with prostatitis syndrome – an evaluation of inflammatory status and search for microorganisms 10 years after
a first analysis. Andrologia. 2003, 35 (5), 258–262. https://www.ncbi.nlm.
nih.gov/pubmed/14535851
Scholes D., Hooton T.M., Roberts P.L., Gupta K., Stapleton A.E., Stamm W.E.: Risk
factors associated with acute pyelonephritis in healthy women. Ann Intern
Med. 2005, 142 (1), 20–27. doi: 10.7326/0003-4819-142-1-200501040-
00008. https://www.ncbi.nlm.nih.gov/pubmed/15630106
Schuts E.C., Hulscher M.E., Mouton J.W., Verduin C.M., Stuart J.W., Overdiek
H.W. i wsp.: Current evidence on hospital antimicrobial stewardship objectives: a systematic review and meta-analysis. Lancet Infect Dis. 2016, 16
(7), 847–856. doi: 10.1016/S1473-3099(16)00065-7. https://www.ncbi.
nlm.nih.gov/pubmed/26947617
Schwenger E.M., Tejani A.M., Loewen P.S.: Probiotics for preventing urinary
tract infections in adults and children. Cochrane Database Syst Rev. 2015,
CD008772. doi: 10.1002/14651858.CD008772.pub2. https://www.ncbi.
nlm.nih.gov/pubmed/26695595
Seyrek M., Binbay M., Yuruk E., Akman T., Aslan R., Yazici O. i wsp.: Perioperative
prophylaxis for percutaneous nephrolithotomy: Randomized study concerning the drug and dosage. J Endourol. 2012, 26 (11), 1431–1436. doi:
10.1089/end.2012.0242. https://www.ncbi.nlm.nih.gov/pubmed/22612061
Sharpe J.R., Sadlowski R.W., Finney R.P., Branch W.T., Hanna J.E.: Urinary
tract infection after transrectal needle biopsy of the prostate. J Urol. 1982,
127 (2), 255–256. doi: 10.1016/s0022-5347(17)53730-1. https://www.ncbi.
nlm.nih.gov/pubmed/7062377
Silver S.A., Baillie L., Simor A.E.: Positive urine cultures: A major cause of inappropriate antimicrobial use in hospitals? Can J Infect Dis Med Microbiol.
2009, 20 (4), 107–111. doi: 10.1155/2009/702545. https://www.ncbi.nlm.
nih.gov/pubmed/21119801
Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D.,
Bauer M. i wsp.: The Third International Consensus Definitions for Sepsis
and Septic Shock (Sepsis-3). JAMA. 2016, 315 (8), 801–810. doi: 10.1001/
jama.2016.0287. https://www.ncbi.nlm.nih.gov/pubmed/26903338
Skerk V., Krhen I., Schonwald S., Cajic V., Markovinovic L., Roglic S. i wsp.: The
role of unusual pathogens in prostatitis syndrome. Int J Antimicrob Agents.
2004, 24 Suppl 1, S53–S56. doi: 10.1016/j.ijantimicag.2004.02.010. https://
www.ncbi.nlm.nih.gov/pubmed/15364308
Skerk V., Schönwald S., Krhen I., Banaszak A., Begovac J., Strugar J. i wsp.:
Comparative analysis of azithromycin and ciprofloxacin in the treatment
of chronic prostatitis caused by Chlamydia trachomatis. Int J Antimicrob
Agents. 2003, 21 (5), 457–462. doi: 10.1016/s0924-8579(03)00056-6.
https://www.ncbi.nlm.nih.gov/pubmed/12727080
Smelov V., Perekalina T., Artemenko N., Smelova N., Ukleeva G., Gorelov A.:
Chlamydia trachomatis survival in the presence of two fluoroquinolones (lomefloxacin versus levofloxacin) in patients with chronic prostatitis syndrome. Andrologia. 2005, 37, 61–64. doi: 10.1111/j.1439-
0272.2005.00654.x. https://www.ncbi.nlm.nih.gov/pubmed/16026425
Sobel J.D., Kauffman C.A., McKinsey D., Zervos M., Vazquez J.A., Karchmer
A.W. i wsp.: Candiduria: a randomized, double-blind study of treatment with
fluconazole and placebo. The National Institute of Allergy and Infectious
Diseases (NIAID) Mycoses Study Group. Clin Infect Dis. 2000, 30 (1), 19–24.
doi: 10.1086/313580. https://www.ncbi.nlm.nih.gov/pubmed/10619727
Sorensen M.D., Krieger J.N.: Fournier’s Gangrene: Epidemiology and
Outcomes in the General US Population. Urol Int. 2016, 97 (3), 249–259.
doi: 10.1159/000445695. https://www.ncbi.nlm.nih.gov/pubmed/27172977
Sousa R., Muñoz-Mahamud E., Quayle J., Dias da Costa L., Casals C., Scott P.: Is
asymptomatic bacteriuria a risk factor for prosthetic joint infection? Clin
Inf Dis. 2014, 59 (1), 41–47. doi: 10.1093/cid/ciu235. https://www.ncbi.
nlm.nih.gov/pubmed/24723280
Spoorenberg V., Hulscher M.E., Akkermans R.P., Prins J.M., Geerlings S.E.:
Appropriate antibiotic use for patients with urinary tract infections reduces
length of hospital stay. Clin Infect Dis. 2014, 58 (2), 164–169. doi: 10.1093/
cid/cit688. https://www.ncbi.nlm.nih.gov/pubmed/24158412
Spoorenberg V., Hulscher M.E., Geskus R.B., de Reijke T.M., Opmeer B.C., Prins
J.M. i wsp.: [Better antibiotic use in complicated urinary tract infections;
multicentre cluster randomised trial of 2 improvement strategies]. Ned
Tijdschr Geneeskd. 2016, 160, D460. https://www.ncbi.nlm.nih.gov/
pubmed/27438395
Stamm W.E., Hooton T.M.: Management of urinary tract infections
in adults. N Engl J Med. 1993, 329 (18), 1328–1334. doi: 10.1056/
NEJM199310283291808. https://www.ncbi.nlm.nih.gov/pubmed/8413414
Stevens D.L., Bisno A.L., Chambers H.F., Dellinger E.P., Goldstein E.J., Gorbach
S.L. i wsp.: Practice guidelines for the diagnosis and management of skin
and soft tissue infections: 2014 update by the infectious diseases society
of America. Clin Infect Dis. 2014, 59 (2), 147–159. doi: 10.1093/cid/ciu296.
https://www.ncbi.nlm.nih.gov/pubmed/24947530
Stothers L.: A randomized trial to evaluate effectiveness and cost effectiveness of naturopathic cranberry products as prophylaxis against urinary
tract infection in women. Can J Urol. 2002, 9 (3), 1558–1562. https://www.
ncbi.nlm.nih.gov/pubmed/12121581
Street E.J., Joyce A., Wilson J.: BASHH UK guideline for the management of
epididymo-orchitis, 2010. Int J STD AIDS. 2011, 22 (7), 361–365. doi: 10.1258/
ijsa.2011.011023. https://www.ncbi.nlm.nih.gov/pubmed/21729951
Street E.J., Justice E.D., Kopa Z., Portman M.D., Ross J.D., Skerlev M. i wsp.:
The 2016 European guideline on the management of epididymo-orchitis.
Int J STD AIDS, 2017, 28 (8), 744–749. doi: 10.1177/0956462417699356.
https://www.ncbi.nlm.nih.gov/pubmed/28632112
Subrahmanyam U., Ugane S.P.: Honey dressing beneficial in treatment of
fournier’s gangrene. Indian J Surg. 2004, 66 (2), 75–77. http://citeseerx.
ist.psu.edu/viewdoc/download?doi=10.1.1.554.4604&rep=rep1&type=pdf
Sunden F., Håkansson L., Ljunggren E., Wullt B.: Escherichia coli 83972 bacteriuria protects against recurrent lower urinary tract infections in patients with
incomplete bladder emptying. J Urol. 2010, 184 (1), 179–185. doi: 10.1016/j.
juro.2010.03.024. https://www.ncbi.nlm.nih.gov/pubmed/20483149
Swartz S.L., Kraus S.J., Herrmann K.L., Stargel M.D., Brown W.J., Allen S.D.:
Diagnosis and etiology of nongonococcal urethritis. J Infect Dis. 1978,
138, 445–454. doi: 10.1093/infdis/138.4.445. https://www.ncbi.nlm.nih.
gov/pubmed/213495
Taher Y., Ozen H., Akdogan B., Unal S., Dogan S.: MP48-11 Prospective randomized controlled study to assess the effect of perineal region cleansing with
povidone iodine before transrectal needle biopsy of the prostate on infectious
complications. J Urol. 2015, 193 (45), e598. doi: 10.1016/j.juro.2015.02.1685.
https://www.jurology.com/doi/full/10.1016/j.juro.2015.02.1685
Takenaka A., Hara R., Ishimura T., Fujii T., Jo Y., Nagai A. i wsp.: A prospective
randomized comparison of diagnostic efficacy between transperineal and
transrectal 12-core prostate biopsy. Prostate Cancer Prostatic Dis. 2008,
11 (2), 134–138. doi: 10.1038/sj.pcan.4500985. https://www.ncbi.nlm.
nih.gov/pubmed/17533394
Tandogdu Z., Bartoletti R., Cai T., Çek M., Grabe M., Kulchavenya E.:
Antimicrobial resistance in urosepsis: outcomes from the multinational,
multicenter global prevalence of infections in urology (GPIU) study 2003-
2013. World J Urol. 2016, 34 (8), 1193–1200. doi: 10.1007/s00345-015-
1722-1. https://www.ncbi.nlm.nih.gov/pubmed/26658886
Tanner J., Dumville J.C., Norman G., Fortnam M.: Surgical hand antisepsis to
reduce surgical site infection. Cochrane Database Syst Rev. 2016: CD004288.
doi: 10.1002/14651858.CD004288.pub3. https://www.ncbi.nlm.nih.gov/
pubmed/26799160
Tanner J., Norrie P., Melen K.: Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011, CD004122. doi:
10.1002/14651858.CD004122.pub4. https://www.ncbi.nlm.nih.gov/
pubmed/22071812
Tekdogan U., Tuncel A., Eroglu M., Unsal A., Atan A., Balbay M.: The efficiency
of prophylactic antibiotic treatment in patients without risk factor who
underwent transrectal. Turk Uroloji Dergisi. 2006, 32, 261–267. https://
www.researchgate.net/publication/289651865
Tencer J.: Asymptomatic bacteriuria – a long-term study. Scand J Urol
Nephrol. 1988, 22 (1), 31–34. doi: 10.1080/00365599.1988.11690380.
https://www.ncbi.nlm.nih.gov/pubmed/3387908
Tenke P., Kovacs B., Bjerklund Johansen T.E., Matsumoto T., Tambyah P.A., Naber
K.G. i wsp.: European and Asian guidelines on management and prevention
of catheter-associated urinary tract infections. Int J Antimicrob Agents.
2008, 31 Suppl 1, S68–S78. doi: 10.1016/j.ijantimicag.2007.07.033. https://
www.ncbi.nlm.nih.gov/pubmed/18006279
The ARISE Investigators and the ANZICS Clinical Trials Group. Goal-directed
resuscitation for patients with early septic shock. N Engl J Med. 2014, 371,
1496–1506. doi: 10.1056/NEJMoa1404380. https://www.nejm.org/doi/
full/10.1056/NEJMoa1404380
The PRISM Investigators: Early, Goal-Directed Therapy for Septic Shock
– A Patient-Level Meta-Analysis. N Engl J Med. 2017, 376, 2223–2234.
doi: 10.1056/NEJMoa1701380. https://www.nejm.org/doi/full/10.1056/
NEJMoa1701380
Thompson P.M., Pryor J.P., Williams J.P., Eyers D.E., Dulake C., Scully M.F.
i wsp.: The problem of infection after prostatic biopsy: The case for the transperineal approach. Br J Urol. 1982, 54 (6), 736–740. doi: 10.1111/j.1464-
410x.1982.tb13637.x. https://www.ncbi.nlm.nih.gov/pubmed/7150932
Thomsen A.C., Mørup L., Hansen K.B.: Antibiotic elimination of group-B streptococci in urine in prevention of preterm labour. Lancet. 1987, 1, 591–
593. doi: 10.1016/s0140-6736(87)90234-0. https://www.ncbi.nlm.nih.
gov/pubmed/2881132
Thoumsin H., Aghayan M., Lambotte R.: Single dose fosfomycin trometamol
versus multiple dose nitrofurantoin in pregnant women with bacteriuria:
preliminary results. Infection. 1990, 18 Suppl 2, S94–S97. doi: 10.1007/
bf01643435. https://www.ncbi.nlm.nih.gov/pubmed/2286469
Trautner B.W.: Asymptomatic bacteriuria: when the treatment is worse than
the disease. Nat Rev Urol. 2011, 9 (2), 85–93. doi: 10.1038/nrurol.2011.192.
https://www.ncbi.nlm.nih.gov/pubmed/22143416
Turner J.A., Ciol M.A., Von Korff M., Berger R.: Validity and responsiveness
of the national institutes of health chronic prostatitis symptom index. J
Urol. 2003, 169 (2), 580–583. doi: 10.1097/01.ju.0000047620.95034.a5.
https://www.ncbi.nlm.nih.gov/pubmed/12544311
Tuzel E., Aktepe O.C., Akdogan B.: Prospective comparative study of two protocols of antibiotic prophylaxis in percutaneous nephrolithotomy. J Endourol.
2013, 27 (2), 172–176. doi: 10.1089/end.2012.0331. https://www.ncbi.nlm.
nih.gov/pubmed/22908891
U.S. Department of Health and Human Services, FDA, Center for Drug
Evaluation and Research (CDER). Complicated Urinary Tract Infections:
Developing Drugs for Treatment Guidance for Industry 2018. https://www.
fda.gov/downloads/Drugs/Guidances/ucm070981.pdf
U.S. Department of Health and Human Services, FDA, Center for Drug
Evaluation and Research (CDER). Uncomplicated Urinary Tract Infections:
Developing Drugs for Treatment. 2015. http://www.fda.gov/Drugs/
GuidanceComplianceRegulatoryInformation/Guidances/default.htm
Ulleryd P., Sandberg T.: Ciprofloxacin for 2 or 4 weeks in the treatment of febrile
urinary tract infection in men: a randomized trial with a 1 year follow-up.
Scand J Infect Dis. 2003, 35 (1), 34–39. doi: 10.1080/0036554021000026988.
https://www.ncbi.nlm.nih.gov/pubmed/12685882
van Buul L.W., Vreeken H.L., Bradley S.F., Crnich C.J., Drinka P.J., Geerlings
S.E. i wsp.: The Development of a Decision Tool for the Empiric Treatment of
Suspected Urinary Tract Infection in Frail Older Adults: A Delphi Consensus
Procedure. J Am Med Dir Assoc. 2018, 19 (9), 757–764 doi: 10.1016/j.
jamda.2018.05.001. https://www.ncbi.nlm.nih.gov/pubmed/29910137
van der Starre W.E., van Nieuwkoop C., Paltansing S., van’t Wout J.W., Groeneveld
G.H., Becker M.J. i wsp.: Risk factors for fluoroquinolone-resistant Escherichia
coli in adults with community-onset febrile urinary tract infection. J
Antimicrob Chemother. 2011, 66 (3), 650–656. doi: 10.1093/jac/dkq465.
https://www.ncbi.nlm.nih.gov/pubmed/21123286
van Haarst, E.P., van Andel G., Heldeweg E.A., Schlatmann T.J., van der Horst
H.J.: Evaluation of the diagnostic workup in young women referred for
recurrent lower urinary tract infections. Urology. 2001, 57 (6), 1068–
1072. doi: 10.1016/s0090-4295(01)00971-2. https://www.ncbi.nlm.nih.
gov/pubmed/23867306
van Nieuwkoop C., Hoppe B.P., Bonten T.N., Van’t Wout J.W., Aarts N.J., Mertens
B.J. i wsp.: Predicting the need for radiologic imaging in adults with febrile
urinary tract infection. Clin Infect Dis. 2010, 51 (11), 1266–1272. doi:
10.1086/657071. https://www.ncbi.nlm.nih.gov/pubmed/21034195
Vazquez J.C., Villar J.: Treatments for symptomatic urinary tract infections during pregnancy. Cochrane Database Syst Rev. 2000, CD002256.
doi: 10.1002/14651858.CD002256. https://www.ncbi.nlm.nih.gov/
pubmed/10908537
Vickovic N., Skerk V., Granic J., Vargovic M., Pasini M., Turcic P.: Metronidazole
1.5 gram dose for 7 or 14 days in the treatment of patients with chronic prostatitis caused by Trichomonas vaginalis: A randomized study. J Chemother.
2010, 22 (5), 364–365. doi: 10.1179/joc.2010.22.5.364. https://www.ncbi.
nlm.nih.gov/pubmed/21123162
Wagenlehner F.M., Hoyme U., Kaase M., Fünfstück R., Naber K.G., Schmiemann
G.: Uncomplicated urinary tract infections. Dtsch Arztebl Int. 2011, 108
(24), 415–423. doi: 10.3238/arztebl.2011.0415. https://www.ncbi.nlm.
nih.gov/pubmed/21776311
Wagenlehner F.M., Naber K.G.: Prostatitis: the role of antibiotic treatment.
World J Urol. 2003, 21 (2), 105–108. doi: 10.1007/s00345-003-0333-4.
https://www.ncbi.nlm.nih.gov/pubmed/12687400
Wagenlehner F.M., Pilatz A., Bschleipfer T., Diemer T., Linn T., Meinhardt A.
i wsp.: Bacterial prostatitis. World J Urol. 2013, 31 (4), 711–716. doi: 10.1007/
s00345-013-1055-x. https://www.ncbi.nlm.nih.gov/pubmed/23519458
Wagenlehner F., Tandogdu Z., Bartoletti R., Cai T., Cek M., Kulchavenya E.
i wsp.: The Global Prevalence of Infections in Urology Study: A Long-Term,
Worldwide Surveillance Study on Urological Infections. Pathogens. 2016,
5 (1). doi: 10.3390/pathogens5010010. https://www.ncbi.nlm.nih.gov/
pubmed/26797640
Wagenlehner F.M., Vahlensieck W., Bauer H.W., Weidner W., Piechota H.J., Naber
K.G.: Prevention of recurrent urinary tract infections. Minerva Urol Nefrol.
2013, 65 (1), 9–20. https://www.ncbi.nlm.nih.gov/pubmed/23538307
Wagenlehner F.M., Wullt B., Perletti G.: Antimicrobials in urogenital infections. Int J Antimicrob Agents. 2011, 38 Suppl, 3–10. doi: 10.1016/j.ijantimicag.2011.09.004. https://www.ncbi.nlm.nih.gov/pubmed/22019184
Walker J.T., Singla N., Roehrborn C.G.: Reducing Infectious Complications
Following Transrectal Ultrasound-guided Prostate Biopsy: A Systematic
Review. Rev Urol. 2016, 18 (2), 73–89. doi: 10.3909/riu0713. https://www.
ncbi.nlm.nih.gov/pubmed/27601966
Wang H., Zhou X., Chen S., Zhu C., Yu X.: Investigation of infection risk and
the value of antibiotic prophylaxis during transrectal biopsy of the prostate
by endotoxin determination. Zhonghua Nan Ke Xue. 2004, (7) 10, 496–498.
https://www.ncbi.nlm.nih.gov/pubmed/15354517
Warren J.W., Abrutyn E., Hebel J.R., Johnson J.R., Schaeffer A.J., Stamm W.E.
i wsp.: Guidelines for antimicrobial treatment of uncomplicated acute bacterial
cystitis and acute pyelonephritis in women. Infectious Diseases Society of
America (IDSA). Clin Infect Dis. 1999, 29 (4), 745–758. doi: 10.1086/520427.
https://www.ncbi.nlm.nih.gov/pubmed/10589881
Warren J.W., Damron D., Tenney J.H., Hoopes J.M., Deforge B., Muncie H.L
Jr.: Fever, bacteremia, and death as complications of bacteriuria in women
with long-term urethral catheters. J Infect Dis. 1987, 155 (6), 1151–
1158. doi: 10.1093/infdis/155.6.1151. https://www.ncbi.nlm.nih.gov/
pubmed/3572035
Warren J.W., Tenney J.H., Hoopes J.M., Muncie H.L., Anthony W.C.: A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982, 146 (6), 719–723. doi: 10.1093/
infdis/146.6.719. https://www.ncbi.nlm.nih.gov/pubmed/6815281
Webster J., Alghamdi A.: Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev. 2015: CD006353.
doi: 10.1002/14651858.CD006353.pub4. https://www.ncbi.nlm.nih.gov/
pubmed/25901509
Webster J., Osborne S.: Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2015:
CD004985. doi: 10.1002/14651858.CD004985.pub5. https://www.ncbi.
nlm.nih.gov/pubmed/25927093
Wetmore C.M., Manhart L.E., Lowens M.S., Golden M.R., Whittington W.L., XetMull A.M. i wsp.: Demographic, behavioral, and clinical characteristics of men
with nongonococcal urethritis differ by etiology: a case-comparison study. Sex
Transm Dis. 2011, 38 (3), 180–186. doi: 10.1097/OLQ.0b013e3182040de9.
https://www.ncbi.nlm.nih.gov/pubmed/21285914
Whalley P.J., Cunningham F.G.: Short-term versus continuous antimicrobial
therapy for asymptomatic bacteriuria in pregnancy. Obstet Gynecol. 1977,
49 (3), 262–265. https://www.ncbi.nlm.nih.gov/pubmed/320525
WHO. Antimicrobial resistance: global report on surveillance 2014. http://
www.who.int/drugresistance/documents/surveillancereport/en/
Widmer M., Lopez I., Gülmezoglu A.M., Mignini L., Roganti A.: Duration of treatment for asymptomatic bacteriuria during pregnancy. Cochrane Database
Syst Rev, 2015: CD000491. doi: 10.1002/14651858.CD000491.pub3. https://
www.ncbi.nlm.nih.gov/pubmed/26560337
Williams G.L., Campbell H., Davies K.J.: Urinary concentrating ability in
women with asymptomatic bacteriuria in pregnancy. Br Med J. 1969, 3,
212–215. doi: 10.1136/bmj.3.5664.212. https://www.ncbi.nlm.nih.gov/
pubmed/5792611
Wilson M.L., Mithecll M., Morris A.J., Murray P.R., Reimer L.G., Reller L.B.
i wsp.: Principles and rocedures for blood cultures; Approved Guideline.
Clinical and Laboratory Standards Institute (CLSI), 2007. https://clsi.org/
media/1448/m47a_sample.pdf
Wing D.A., Hendershott C.M., Debuque L., Millar L.K.: A randomized trial of
three antibiotic regimens for the treatment of pyelonephritis in pregnancy.
Obstet Gynecol. 1998, 92 (2), 249–253. doi: 10.1016/s0029-7844(98)00156-
2. https://www.ncbi.nlm.nih.gov/pubmed/9699761
Wise G.J., Shteynshlyuger A.: Atypical infections of the prostate. Curr
Prostate Rep. 2008, 6, 86–93. https://link.springer.com/article/10.1007/
s11918-008-0014-2
Witkin S.S., Jeremias J., Toth M., Ledger W.J.: Detection of Chlamydia trachomatis by the polymerase chain reaction in the cervices of women
with acute salpingitis. Am J Obstet Gynecol. 1993, 168 (5), 1438–1442.
doi: 10.1016/s0002-9378(11)90778-9. https://www.ncbi.nlm.nih.gov/
pubmed/8498424
Workowski K.A., Bolan G.A.: Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015, 64, 1–137. https://www.ncbi.nlm.
nih.gov/pubmed/26042815
Workowski K.A., Bolan G.A.: Sexually transmitted disease treatment
guidelines. Center for Disease Contol, 2015. MMWR Recomm Rep. 2015,
64 (RR-03), 1–137. PMID: 26042815. https://pubmed.ncbi.nlm.nih.
gov/26042815-sexually-transmitted-diseases-treatment-guidelines-2015/
Workshop Committee of the National Institute of Diabetes and Digestive
and Kidney Disease (NIDDK). Chronic prostatitis workshop. 1995: Bethesda,
Maryland.
Wren B.G.: Subclinical renal infection and prematurity. Med J Aust. 1969,
2, 596–600. https://www.ncbi.nlm.nih.gov/pubmed/5388374
Wullt B., Agace W., Mansson W.: Bladder, bowel and bugs – bacteriuria in
patients with intestinal urinary diversion. World J Urol. 2004, 22 (3), 186–
195. doi: 10.1007/s00345-004-0432-x. https://www.ncbi.nlm.nih.gov/
pubmed/15309491
Yamamoto S., Ishitoya S., Segawa T., Kamoto T., Okumura K., Ogawa O.:
Antibiotic prophylaxis for transrectal prostate biopsy: A prospective randomized study of tosufloxacin versus levofloxacin. Int J Urol. 2008, 15 (7),
604–606. doi: 10.1111/j.1442-2042.2008.02056.x. https://www.ncbi.nlm.
nih.gov/pubmed/18462354
Yang L., Hu J., Wei H., Wang L., Zhong H.: Clinical significance of antibiotic prophylaxis for transrectal prostate biopsy. Zhonghua Wai Ke Za Zhi.
2001, 39 (12), 940–942. https://www.ncbi.nlm.nih.gov/pubmed/16201177
Yoon B.I., Kim S., Han D.S., Ha U.S., Lee S.J., Kim H.W. i wsp.: Acute bacterial
prostatitis: how to prevent and manage chronic infection? J Infect Chemother.
2012, 18 (4), 444–450. doi: 10.1007/s10156-011-0350-y. https://www.ncbi.
nlm.nih.gov/pubmed/22215226
You C., Hamasuna R., Ogawa M., Fukuda K., Hachisuga T., Matsumoto T. i wsp.:
The first report: An analysis of bacterial flora of the first voided urine specimens of patients with male urethritis using the 16S ribosomal RNA genebased clone library method. Microb Pathog. 2016, 95, 95–100. doi: 10.1016/j.
micpath.2016.02.022. https://www.ncbi.nlm.nih.gov/pubmed/27013259
Yuan Z., He C., Yan S., Ke Y., Tang W.: Randomized controlled clinical trial on
the efficacy of fosfomycin trometamol for uncomplicated gonococcal urethritis in men. Clin Microbiol Infect. 2016, 22 (6), 507–512. doi: 10.1016/j.
cmi.2016.03.031. https://www.ncbi.nlm.nih.gov/pubmed/27064136
Yu L., Ma L., Yu H.: Impact of insertion timing of iodophor cotton ball on
the control of infection complications after transrectal ultrasound guided
prostate biopsy. Nat Med J China. 2014, 94 (8), 609–611. https://www.
ncbi.nlm.nih.gov/pubmed/24762693
Zani E.L., Clark O.A., Rodrigues Netto N. Jr.: Antibiotic prophylaxis for transrectal prostate biopsy. Cochrane database of systematic reviews, 2011. 11:
CD006576. doi: 10.1002/14651858.CD006576.pub2. https://www.ncbi.
nlm.nih.gov/pubmed/21563156
Zegarra Montes L.Z., Sanchez Mejia A.A., Loza Munarriz C.A., Gutierrez E.C.:
Semen and urine culture in the diagnosis of chronic bacterial prostatitis. Int
Braz J Urol. 2008, 34 (1), 30–37. doi: 10.1590/s1677-55382008000100006.
https://www.ncbi.nlm.nih.gov/pubmed/18341719
Zermann D.H., Ishigooka M., Doggweiler R., Schmidt R.A.: Neurourological
insights into the etiology of genitourinary pain in men. J Urol. 1999, 161
(3), 903–908. https://www.ncbi.nlm.nih.gov/pubmed/10022711
Zhanel G.G., Harding G.K., Nicolle L.E.: Asymptomatic bacteriuria in patients
with diabetes mellitus. Rev Infect Dis. 1991, 13 (1), 150–154. doi: 10.1093/
clinids/12.5.150. https://www.ncbi.nlm.nih.gov/pubmed/2017615
REKOMENDACJE DOTYCZĄCE POSTĘPOWANIA
W ZABURZENIACH SEKSUALNYCH U MĘŻCZYZN
GUIDELINES ON MALE SEXUAL DYSFUNCTION:
ERECTILE DYSFUNCTION AND PREMATURE EJACULATION
REKOMENDACJE DOTYCZĄCE POSTĘPOWANIA
W ZABURZENIACH SEKSUALNYCH U MĘŻCZYZN
GUIDELINES ON MALE SEXUAL DYSFUNCTION:
ERECTILE DYSFUNCTION AND PREMATURE EJACULATION
K. Hatzimouratidis (przewodniczący), F. Giuliano, I. Moncada, A. Muneer, A. Salonia, P. Verze,
A. Parnham, E.C. Serefoglu
Tłumaczenie i przygotowanie wersji polskiej / Translation and elaboration of Polish version:
Marta Sochaj1, Jolanta Słowikowska-Hilczer2
1 Katedra Humanizacji Medycyny i Seksuologii, Uniwersytet Zielonogórski; 2 Zakład Endokrynologii Płodności, Katedra Andrologii
i Endokrynologii Płodności, Uniwersytet Medyczny w Łodzi
Autor do korespondencji / corresponding author:
Jolanta Słowikowska-Hilczer, Zakład Endokrynologii Płodności, Katedra Andrologii i Endokrynologii Płodności, Uniwersytet Medyczny
w Łodzi, ul. Pomorska 251. 92-213 Łódź, tel.: 42 201-41-42, jolanta.slowikowska-hilczer@umed.lodz.pl
Otrzymano/received: 25.11.2019 r. Zaakceptowano/accepted: 27.12.2019 r.
DOI: 10.26404/PAO_2353-8791.2019.07
Skróty / Abbreviations
AUC – pole powierzchni pod krzywą (ang. area under the curve); CHF – zastoinowa niewydolność serca (ang. congestive heart failure);
Cmax – maksymalne stężenie leku, jakie jest osiągane we krwi po podaniu (ang. maximal concentration); ED – zaburzenia erekcji (ang.
erectile dysfunction); EKG – elektrokardiogram (ang. electrocardiography); IELT – wewnątrzpochwowy czas opóźnienia ejakulacji
(ang. intravaginal ejaculatory latency time); EMA – Europejska Agencja Leków (ang. European Medicines Agency); IIEF – międzynarodowy indeks funkcji erekcyjnej (ang. international index of erectile function); LE – poziom wiarygodności dowodu naukowego
(ang. level of evidence); LVD – niewydolność lewej komory serca (ang. left ventricular dysfunction; NTPR – nocna ocena sztywności
i twardości prącia (ang. nocturnal penile tumescence and rigidity); NYHA – Nowojorskie Towarzystwo Chorób Serca (ang. New York
Heart Association); PE – przedwczesny wytrysk (ang. premature ejaculation); PDE5i – inhibitory fosfodiesterazy 5 (ang. phosphodiesterase 5 inhibitors); PRO – raport pacjenta (ang. patient-reported outcome); RP – radykalne wycięcie gruczołu krokowego (ang. radical
prostatectomy); SSRI – inhibitory wychwytu zwrotnego serotoniny (ang. selective serotonin re-uptake inhibitor); T½ – biologiczny
okres półtrwania leku, czas, w którym stężenie leku we krwi zmniejszy się do połowy wartości początkowej (ang. plasma elimination
halftime); Tmax – czas, który mija od podania leku do osiągnięcia; USG – ultrasonografia (ang. ultrasonography)
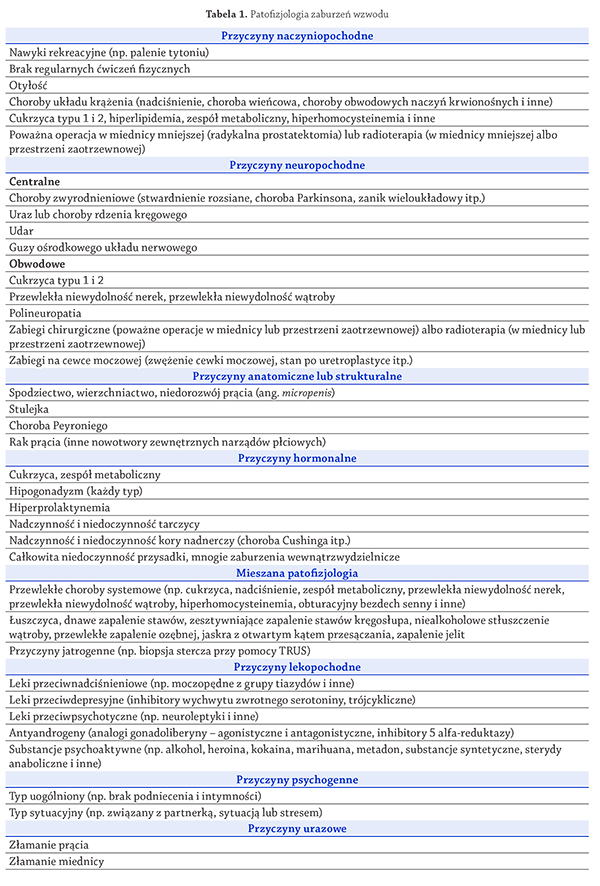
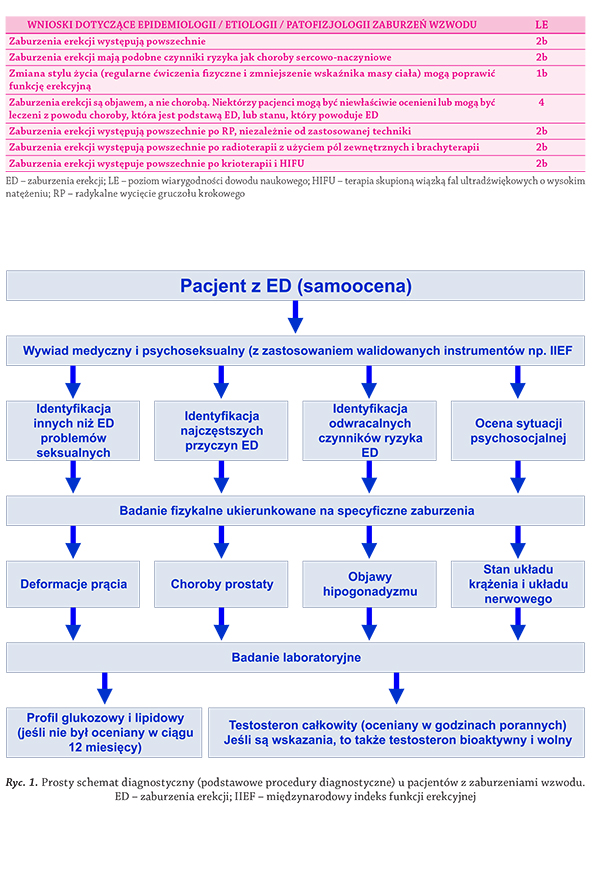
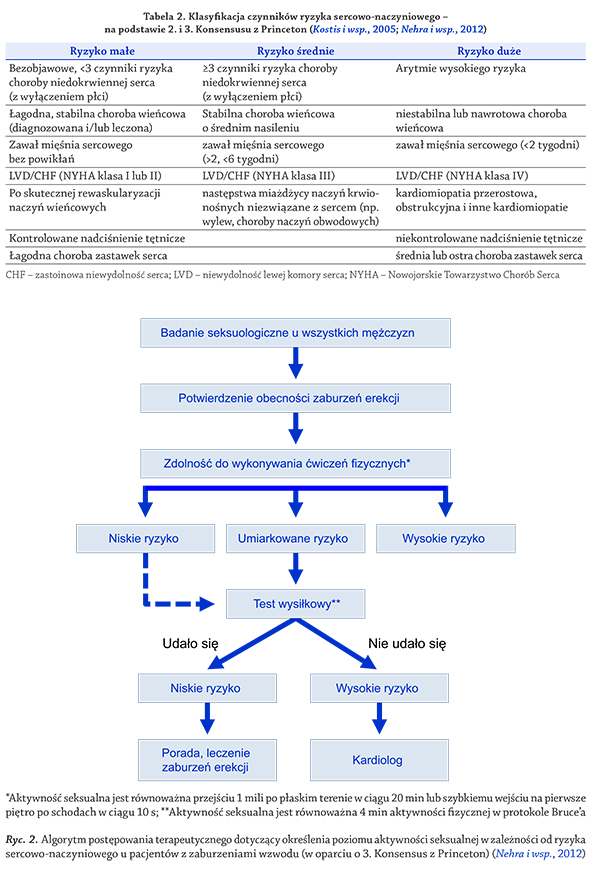
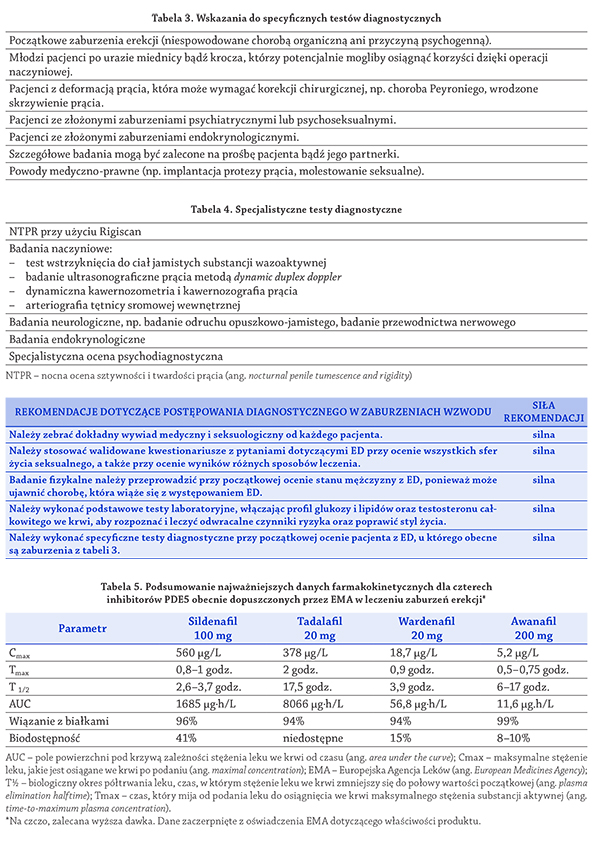
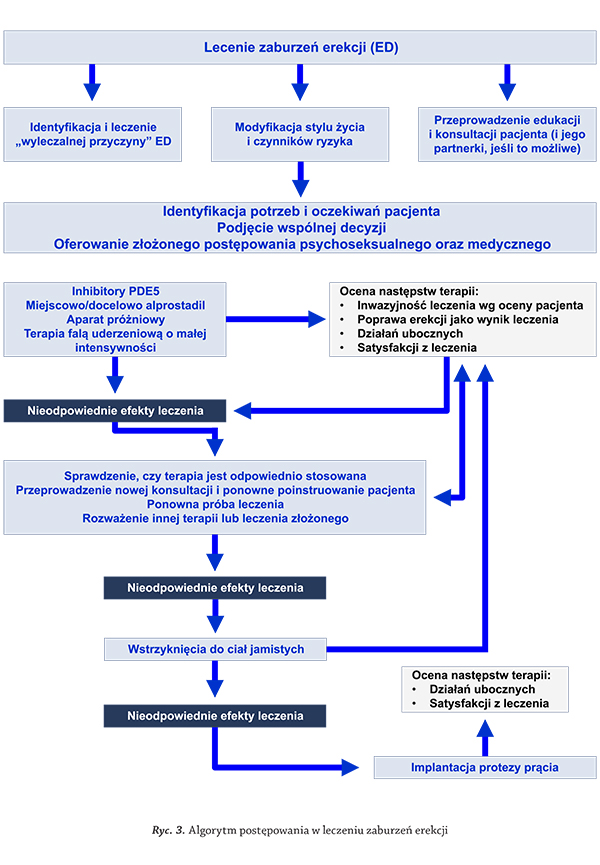
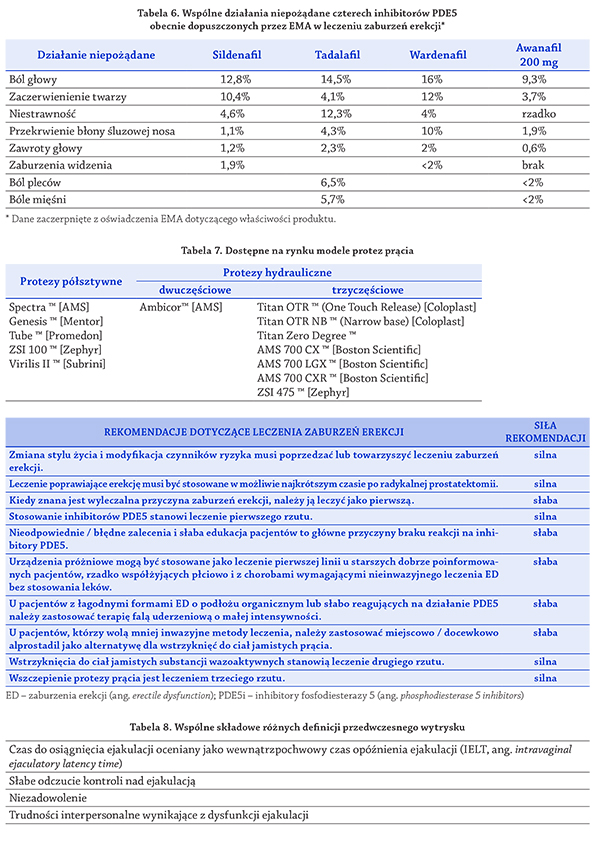
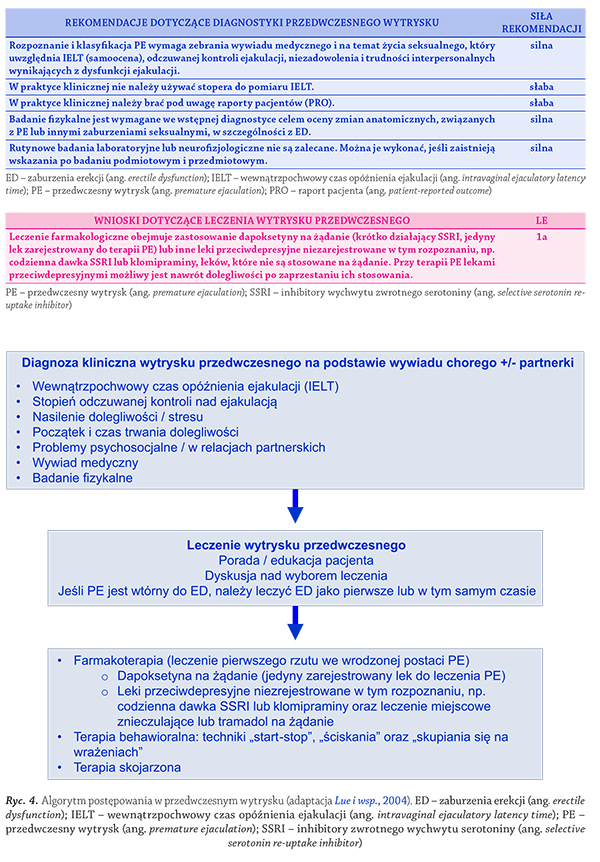
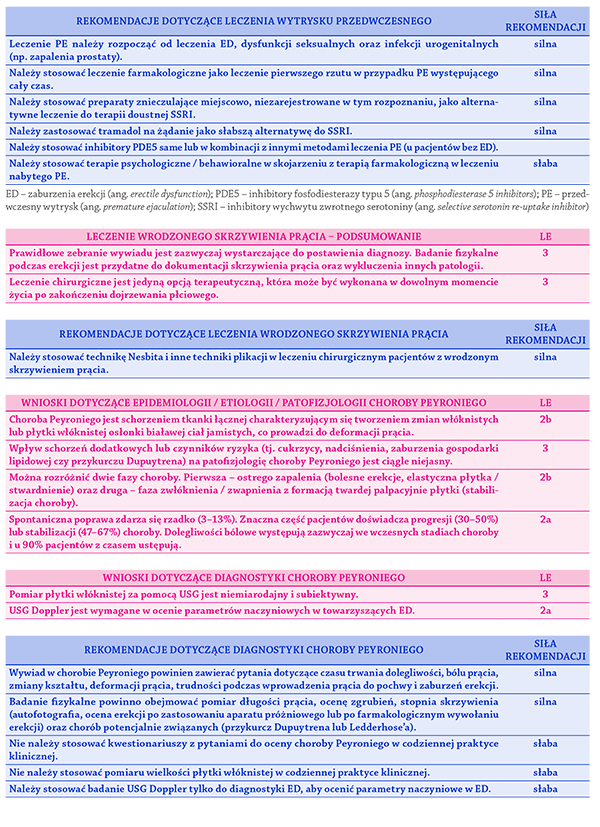
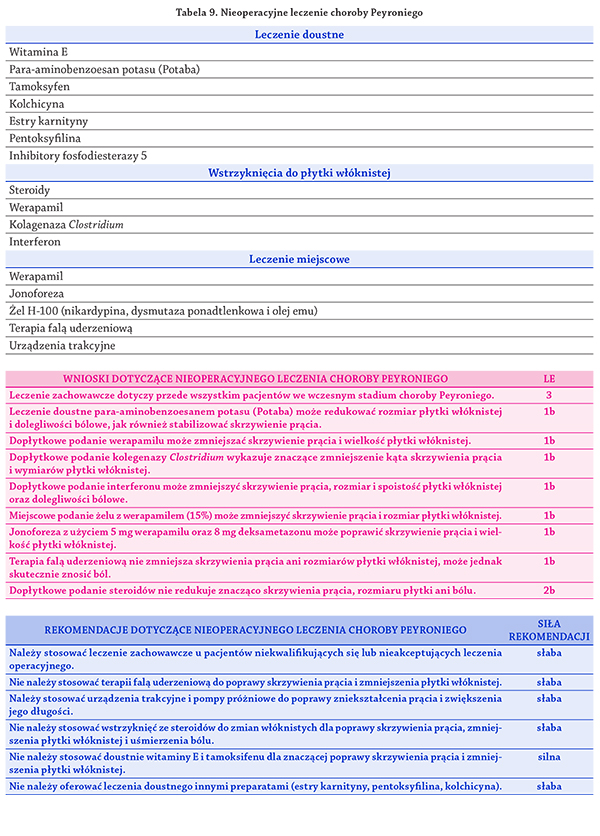
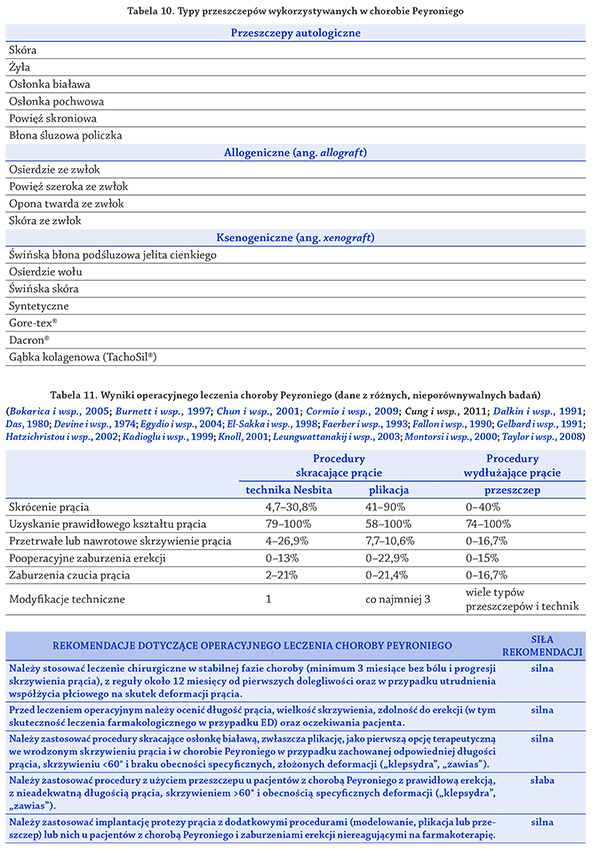
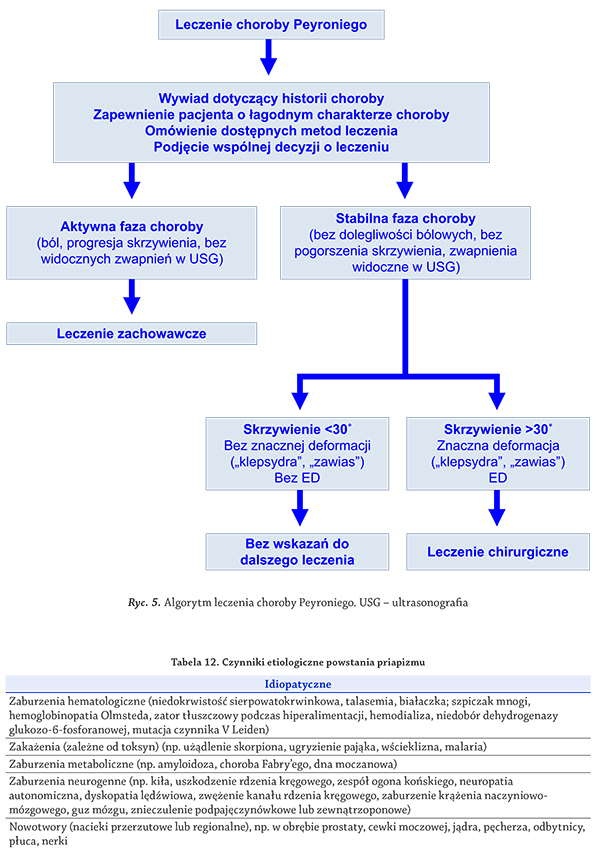
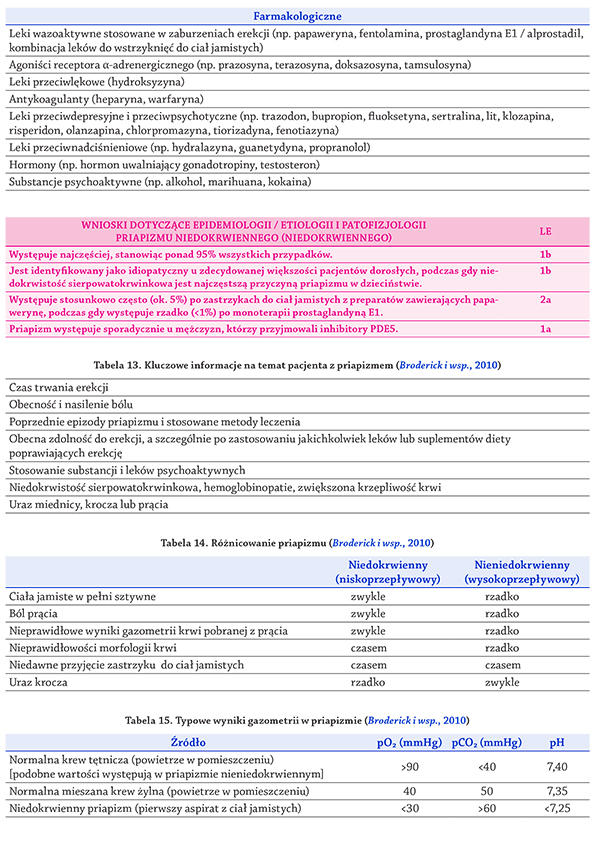
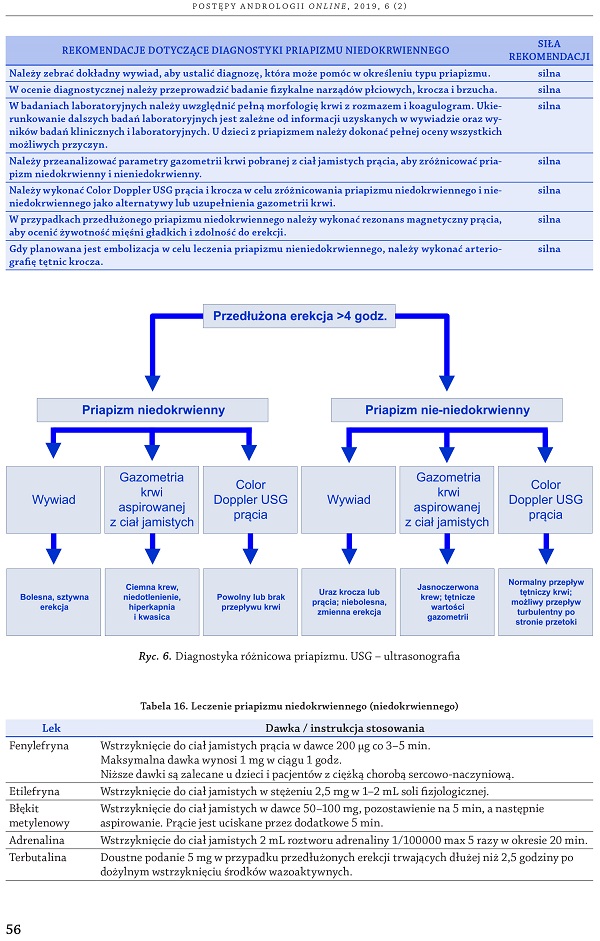
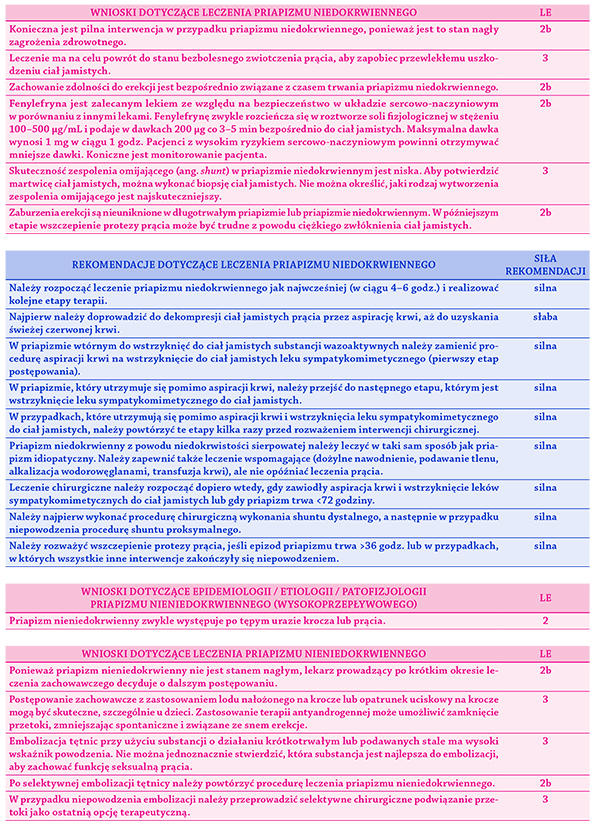
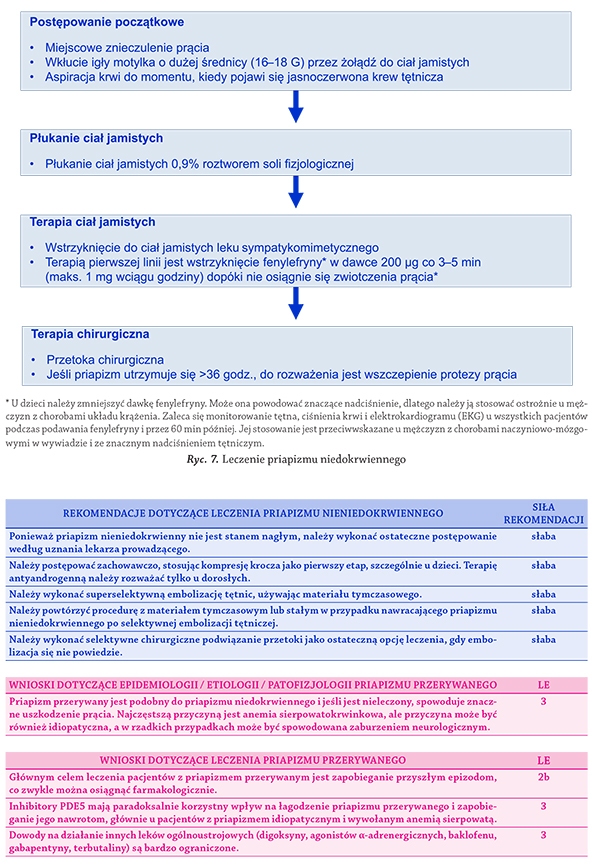
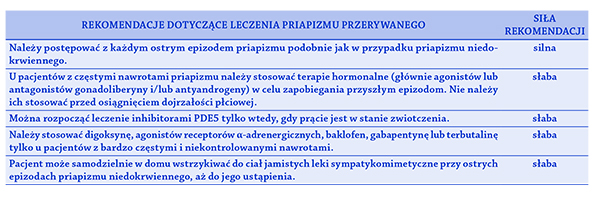
Piśmiennictwo
Piśmiennictwo
Abdel-Hamid I.A., El Naggar E.A., El Gilany A.H.: Assessment of as needed use
of pharmacotherapy and the pause-squeeze technique in premature ejaculation. Int J Impot Res. 2001, 13 (1), 41–45. doi: 10.1038/sj.ijir.3900630.
https://www.ncbi.nlm.nih.gov/pubmed/11313839
Abner E.L., Schmitt F.A., Mendiondo M.S., Marcum J.L., Kryscio R.J.: Vitamin
E and all-cause mortality: a meta-analysis. Curr Aging Sci. 2011, 4 (2),
158–170. doi: 10.2174/1874609811104020158. https://www.ncbi.nlm.
nih.gov/pubmed/21235492
Abu El-Hamd M., Abdelhamed A.: Comparison of the clinical efficacy and safety
of the on-demand use of paroxetine, dapoxetine, sildenafil and combined
dapoxetine with sildenafil in treatment of patients with premature ejaculation: A randomised placebo-controlled clinical trial. Andrologia. 2018, 50 (1).
doi: 10.1111/and.12829. https://www.ncbi.nlm.nih.gov/pubmed/28497478
Adeyoju A.B., Olujohungbe A.B., Morris J., Yardumian A., Bareford D., Akenova
A. i wsp.: Priapism in sickle-cell disease; incidence, risk factors and complications – an international multicentre study. BJU Int. 2002, 90 (9), 898–
902. doi: 10.1046/j.1464-410x.2002.03022.x. https://www.ncbi.nlm.nih.
gov/pubmed/12460353
Akakpo W., Pineda M.A., Burnett A.L.: Critical Analysis of Satisfaction
Assessment After Penile Prosthesis Surgery. Sex Med Rev. 2017, 5 (2),
244–251. doi: 10.1016/j.sxmr.2017.01.001. https://www.ncbi.nlm.nih.
gov/pubmed/28143706
Akkus E., Carrier S., Rehman J., Breza J., Kadioglu A., Lue T.F.: Is colchicine
effective in Peyronie’s disease? A pilot study. Urology. 1994, 44 (2), 291–
295. doi: 10.1016/s0090-4295(94)80155-x. https://www.ncbi.nlm.nih.
gov/pubmed/8048212
Akman T., Sanli O., Uluocak N., Akbulut F., Nane I., Demir S. i wsp.: The most
commonly altered type of Peyronie’s disease deformity under oral colchicine treatment is lateral curvature that mostly shifts to the dorsal side.
Andrologia. 2011, 43 (1), 28–33. doi: 10.1111/j.1439-0272.2009.01004.x.
https://www.ncbi.nlm.nih.gov/pubmed/21219379
Alberti L., Torlasco C., Lauretta L., Loffi M., Maranta F., Salonia A. i wsp.: Erectile
dysfunction in heart failure patients: a critical reappraisal. Andrology. 2013,
1 (2), 177–191. doi: 10.1111/j.2047-2927.2012.00048.x. https://www.ncbi.
nlm.nih.gov/pubmed/23339018
Alexander Tonseth K., Egge T., Kolbenstvedt A., Hedlund H.: Evaluation of patients
after treatment of arterial priapism with selective micro-embolization. Scand
J Urol Nephrol. 2006, 40 (1), 49–52. doi: 10.1080/00365590500338040.
https://www.ncbi.nlm.nih.gov/pubmed/16452056
Althof S.E.: Prevalence, characteristics and implications of premature ejaculation/rapid ejaculation. J Urol. 2006, 175, 842–848. doi: 10.1016/S0022-
5347(05)00341-1. https://www.ncbi.nlm.nih.gov/pubmed/16469562
Althof S.E., Abdo C.H., Dean J., Hackett G., McCabe M., McMahon C.G. i wsp.:
International Society for Sexual Medicine’s guidelines for the diagnosis and
treatment of premature ejaculation. J Sex Med. 2010, 7, (9), 2947–2969.
doi: 10.1111/j.1743-6109.2010.01975.x. https://www.ncbi.nlm.nih.gov/
pubmed/21050394
Althof S.E., McMahon C.G., Waldinger M.D., Serefoglu E.C., Shindel A.W., Adaikan
P.G. i wsp.: An update of the International Society of Sexual Medicine’s
guidelines for the diagnosis and treatment of premature ejaculation (PE).
J Sex Med. 2014 (6), 11, 1392–1422. doi: 10.1111/jsm.12504. https://www.
ncbi.nlm.nih.gov/pubmed/24848686
Althof S.E., Rosen R.C., Perelman M.A., Rubio-Aurioles E.: Standard operating procedures for taking a sexual history. J Sex Med. 2013, 10 (1), 26–35.
doi: 10.1111/j.1743-6109.2012.02823.x. https://www.ncbi.nlm.nih.gov/
pubmed/22970717
Althof S., Rosen R., Symonds T., Mundayat R., May K., Abraham L.: Development
and validation of a new questionnaire to assess sexual satisfaction, control,
and distress associated with premature ejaculation. J Sex Med. 2006, 3 (3),
465–475. doi: 10.1111/j.1743-6109.2006.00239.x. https://www.ncbi.nlm.
nih.gov/pubmed/16681472
Althof S.E., Symonds T.: Patient reported outcomes used in the assessment of premature ejaculation. Urol Clin North Am. 2007, 34 (4), 581–
589. doi: 10.1016/j.ucl.2007.08.001. https://www.ncbi.nlm.nih.gov/
pubmed/17983898
Alwaal A., Al-Mannie R., Carrier S.: Future prospects in the treatment of erectile
dysfunction: focus on avanafil. Drug Des Devel Ther. 2011, 5, 435–443. doi:
10.2147/DDDT.S15852. https://www.ncbi.nlm.nih.gov/pubmed/22087063
American Psychiatric Association., Diagnostic and Statistical Manual of
Mental Disorders. 4th edn. Text Revision. [Access date February 2014]
Revision. 2000, American Psychiatric Publishing Inc: Washington, DC. http://
dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596
Anaissie J., Hellstrom W.J.: Clinical use of alprostadil topical cream in patients
with erectile dysfunction: a review. Res Rep Urol. 2016, 8, 123–131. doi:
10.2147/RRU.S68560. https://www.ncbi.nlm.nih.gov/pubmed/27536559
Anderson M.S., Shankey T.V., Lubrano T., Mulhall J.P.: Inhibition of Peyronie’s
plaque fibroblast proliferation by biologic agents. Int J Impot Res. 2000,
12 Suppl 3, S25–S31. doi: 10.1038/sj.ijir.3900558. https://www.ncbi.nlm.
nih.gov/pubmed/11002396
Antonini G., Busetto G.M., De Berardinis E., Giovannone R., Vicini P., Del Giudice
F. i wsp.: Minimally invasive infrapubic inflatable penile prosthesis implant
for erectile dysfunction: Evaluation of efficacy, satisfaction profile and complications. Int J Impot Res. 2016, 28 (1), 4–8. doi: 10.1038/ijir.2015.33.
https://www.ncbi.nlm.nih.gov/pubmed/26657316
Arafa M., Eid H., El-Badry A., Ezz-Eldine K., Shamloul R.: The prevalence of
Peyronie’s disease in diabetic patients with erectile dysfunction. Int J Impot
Res. 2007, 19 (2), 213–217. doi: 10.1038/sj.ijir.3901518. https://www.ncbi.
nlm.nih.gov/pubmed/16915304
Arafa M., Shamloul R.: Development and evaluation of the Arabic Index
of Premature Ejaculation (AIPE). J Sex Med. 2007, 4 (6), 1750–1756. doi:
10.1111/j.1743-6109.2006.00213.x. https://www.ncbi.nlm.nih.gov/
pubmed/17970977
Arango O., Castro R., Dominguez J., Gelabert A.: Complete resolution of posttraumatic high-flow priapism with conservative treatment. Int J Impot Res.
1999, 11 (2), 115–117. https://www.ncbi.nlm.nih.gov/pubmed/10356672
Ateyah A., Rahman El-Nashar A., Zohdy W., Arafa M., Saad El-Den H.:
Intracavernosal irrigation by cold saline as a simple method of treating iatrogenic prolonged erection. J Sex Med. 2005, 2 (2), 248–253. doi:
10.1111/j.1743-6109.2005.20235.x. https://www.ncbi.nlm.nih.gov/
pubmed/16422893
Atikeler M.K., Gecit I., Senol F.A.: Optimum usage of prilocaine-lidocaine
cream in premature ejaculation. Andrologia. 2002, 34 (6), 356–359. doi:
10.1046/j.1439-0272.2002.00511.x. https://www.ncbi.nlm.nih.gov/
pubmed/12472618
Bai Y., Pu C., Han P., Li J., Yuan H., Tang Y. i wsp.: Selective Serotonin Reuptake
Inhibitors Plus Phosphodiesterase-5 Inhibitors for Premature Ejaculation:
A Systematic Review and Meta-analysis. Urology. 2015, 86 (4), 758–764.
doi: 10.1016/j.urology.2015.06.045. https://www.ncbi.nlm.nih.gov/
pubmed/26247816
Bailey A.J., Tarlton J.F., Van der Stappen J., Sims T.J., Messina A.: The continuous elongation technique for severe Dupuytren’s disease. A biochemical
mechanism. J Hand Surg Br. 1994, 19 (4), 522–527. doi: 10.1016/0266-
7681(94)90220-8. https://www.ncbi.nlm.nih.gov/pubmed/7964107
Baillargeon J., Urban R.J., Kuo Y.F., Ottenbacher K.J., Raji M.A., Du F. i wsp.: Risk
of Myocardial Infarction in Older Men Receiving Testosterone Therapy. Ann
Pharmacother. 2014, 48 (9), 1138–1144. doi: 10.1177/1060028014539918.
https://www.ncbi.nlm.nih.gov/pubmed/24989174
Ballas S.K., Lyon D.: Safety and efficacy of blood exchange transfusion for
priapism complicating sickle cell disease. J Clin Apher. 2016, 31 (1), 5–10.
doi: 10.1002/jca.21394. https://www.ncbi.nlm.nih.gov/pubmed/25809639
Bar Yosef Y., Binyamini J., Matzkin H., Ben-Chaim J.: Midline dorsal plication technique for penile curvature repair. J Urol. 2004, 172, 1368–1369.
doi: 10.1097/01.ju.0000138341.68365.b6. https://www.ncbi.nlm.nih.gov/
pubmed/15371846
Bar-Or D., Salottolo K.M., Orlando A., Winkler J.V.: A randomized double-blind,
placebo-controlled multicenter study to evaluate the efficacy and safety of
two doses of the tramadol orally disintegrating tablet for the treatment of
premature ejaculation within less than 2 minutes. Eur Urol. 2012, 61 (4),
736–743. doi: 10.1016/j.eururo.2011.08.039. https://www.ncbi.nlm.nih.
gov/pubmed/21889833
Bartolucci P., Galactéros F.: Clinical management of adult sickle-cell
disease. Curr Opin Hematol. 2012, 19 (3), 149–155. doi: 10.1097/
MOH.0b013e328351c35f. https://www.ncbi.nlm.nih.gov/pubmed/22357165
Basaria S., Coviello A.D., Travison T.G., Storer T.W., Farwell W.R., Jette A.M.
i wsp.: Adverse events associated with testosterone administration. N Engl
J Med. 2010, 363 (2), 109–122. doi: 10.1056/NEJMoa1000485. https://
www.ncbi.nlm.nih.gov/pubmed/20592293
Baskin L.S., Duckett J.W., Lue T.F.: Penile curvature. Urology. 1996, 48 (3),
347–356. doi: 10.1016/S0090-4295(96)00213-0. https://www.ncbi.nlm.
nih.gov/pubmed/8804484
Bastuba M.D., Saenz de Tejada I., Dinlenc C., Sarazen A., Krane R.J., Goldstein
I.: Arterial priapism: diagnosis, treatment and long-term followup. J Urol.
1994, 151 (5), 1231–1237. doi: 10.1016/s0022-5347(17)35219-9. https://
www.ncbi.nlm.nih.gov/pubmed/8158765
Bechara A., Casabé A., Chéliz G., Romano S., Rey H., Fredotovich N.: Comparative
study of papaverine plus phentolamine versus prostaglandin E1 in erectile
dysfunction. J Urol. 1997, 157 (6), 2132–2134. https://www.ncbi.nlm.nih.
gov/pubmed/9146599
Bechara A., Casabé A., De Bonis W., Ciciclia P.G.: Twelve-Month Efficacy and
Safety of Low-Intensity Shockwave Therapy for Erectile Dysfunction in
Patients Who Do Not Respond to Phosphodiesterase Type 5 Inhibitors.
Sex Med. 2016, 4 (4), e225–232. doi: 10.1016/j.esxm.2016.06.001. https://
www.ncbi.nlm.nih.gov/pubmed/27444215
Behr-Roussel D., Gorny D., Mevel K., Caisey S., Bernabé J., Burgess G. i wsp.:
Chronic sildenafil improves erectile function and endothelium-dependent cavernosal relaxations in rats: lack of tachyphylaxis. Eur Urol. 2005,
47 (1), 87–91. doi: 10.1016/j.eururo.2004.09.005. https://www.ncbi.nlm.
nih.gov/pubmed/15582254
Bekos A., Arvaniti M., Hatzimouratidis K., Moysidis K., Tzortzis V., Hatzichristou
D.: The natural history of Peyronie’s disease: an ultrasonography-based
study. Eur Urol. 2008, 53 (3), 644–650. doi: 10.1016/j.eururo.2007.07.013.
https://www.ncbi.nlm.nih.gov/pubmed/17673362
Bennett N.E., Guhring P., Mulhall J.P.: Intralesional verapamil prevents
the progression of Peyronie’s disease. Urology. 2007, 69 (6), 1181–1184.
doi: 10.1016/j.urology.2007.02.042. https://www.ncbi.nlm.nih.gov/
pubmed/17572211
Bennett N.E., Mulhall J.P.: Sickle cell disease status and outcomes of AfricanAmerican men presenting with priapism. J Sex Med. 2008, 5 (5), 1244–
1250. doi: 10.1111/j.1743-6109.2008.00770.x. https://www.ncbi.nlm.nih.
gov/pubmed/18312286
Berger R., Billups K., Brock G., Broderick G.A., Dhabuwala C.B., Goldstein I. i wsp.:
Report of the American Foundation for Urologic Disease (AFUD) Thought
Leader Panel for evaluation and treatment of priapism. Int J Impot Res.
2001, 13 Suppl 5, S39–43. doi: 10.1038/sj.ijir.3900777. https://www.ncbi.
nlm.nih.gov/pubmed/11781746
Bertolotto M., Quaia E., Mucelli F.P., Ciampalini S., Forgács B., Gattuccio I. i wsp.:
Color Doppler imaging of posttraumatic priapism before and after selective embolization. Radiographics. 2003, 23 (2), 495–503. doi: 10.1148/
rg.232025077. https://www.ncbi.nlm.nih.gov/pubmed/12640162
Bertolotto M., Zappetti R., Pizzolato R., Liguori G.: Color Doppler appearance of
penile cavernosal-spongiosal communications in patients with high-flow priapism. Acta Radiol. 2008, 49 (6), 710–714. doi: 10.1080/02841850802027026.
https://www.ncbi.nlm.nih.gov/pubmed/18568565
Besiroglu H., Otunctemur A., Ozbek E.: The relationship between metabolic syndrome, its components, and erectile dysfunction: a systematic review and a
meta-analysis of observational studies. J Sex Med. 2015, 12 (6), 1309–1318.
doi: 10.1111/jsm.12885. https://www.ncbi.nlm.nih.gov/pubmed/25872648
Bettocchi C., Palumbo F., Spilotros M., Lucarelli G., Palazzo S., Battaglia M.
i wsp.: Patient and partner satisfaction after AMS inflatable penile prosthesis implant. J Sex Med. 2010, 7, 304–309. doi: 10.1111/j.1743-
6109.2009.01499.x. https://www.ncbi.nlm.nih.gov/pubmed/19758282
Bhasin S., Cunningham G.R., Hayes F.J., Matsumoto A.M., Snyder P.J., Swerdloff
R.S. i wsp.: Testosterone therapy in men with androgen deficiency syndromes:
an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab.
2010, 95 (6), 2536–2559. doi: 10.1210/jc.2009-2354. https://www.ncbi.
nlm.nih.gov/pubmed/20525905
Bhat G.S., Shastry A.: Effectiveness of ‘on demand’ silodosin in the treatment
of premature ejaculation in patients dissatisfied with dapoxetine: a randomized control study. Cent European J Urol. 2016, 69 (3), 280–284. doi:
10.5173/ceju.2016.843. https://www.ncbi.nlm.nih.gov/pubmed/27729995
Biagiotti G., Cavallini G.: Acetyl-L-carnitine vs tamoxifen in the oral therapy
of Peyronie’s disease: a preliminary report. BJU Int. 2001, 88 (1), 63–67.
doi: 10.1046/j.1464-410x.2001.02241.x. https://www.ncbi.nlm.nih.gov/
pubmed/11446848
Binmoammar T.A., Hassounah S., Alsaad S., Rawaf S., Majeed A.: The impact
of poor glycaemic control on the prevalence of erectile dysfunction in men
with type 2 diabetes mellitus: a systematic review. JRSM Open. 2016, 7,
2054270415622602. doi: 10.1177/2054270415622602. https://www.ncbi.
nlm.nih.gov/pubmed/26981254
Bivalacqua T.J., Musicki B., Hsu L.L., Gladwin M.T., Burnett A.L., Champion
H.C.: Establishment of a transgenic sickle-cell mouse model to study the
pathophysiology of priapism. J Sex Med. 2009, 6 (9), 2494–2504. doi:
10.1111/j.1743-6109.2009.01359.x. https://www.ncbi.nlm.nih.gov/
pubmed/19523035
Bivalacqua T.J., Musicki B., Kutlu O., Burnett A.L.: New insights into the pathophysiology of sickle cell disease-associated priapism. J Sex Med. 2012, 9
(1), 79–87. doi: 10.1111/j.1743-6109.2011.02288.x. https://www.ncbi.nlm.
nih.gov/pubmed/21554553
Bjekic M.D., Vlajinac H.D., Sipetic S.B., Marinkovic J.M.: Risk factors for
Peyronie’s disease: a case-control study. BJU Int. 2006, 97 (3), 570–574.
doi: 10.1111/j.1464-410X.2006.05969.x. https://www.ncbi.nlm.nih.gov/
pubmed/16469028
Boddi V., Castellini G., Casale H., Rastrelli G., Boni L., Corona G. i wsp.: An integrated approach with vardenafil orodispersible tablet and cognitive behavioral
sex therapy for treatment of erectile dysfunction: a randomized controlled
pilot study. Andrology. 2015, 3 (5), 909–918. doi: 10.1111/andr.12079.
https://www.ncbi.nlm.nih.gov/pubmed/26311340
Bodner D.R., Lindan R., Leffler E., Kursh E.D., Resnick M.I.: The application
of intracavernous injection of vasoactive medications for erection in men
with spinal cord injury. J Urol. 1987, 138 (2), 310–311. doi: 10.1016/s0022-
5347(17)43130-2. https://www.ncbi.nlm.nih.gov/pubmed/3599245
Bokarica P., Parazajder J., Mazuran B., Gilja I.: Surgical treatment of Peyronie’s
disease based on penile length and degree of curvature. Int J Impot Res.
2005, 17 (2), 170–174. doi: 10.1038/sj.ijir.3901255. https://www.ncbi.nlm.
nih.gov/pubmed/15215882
Bolat D., Kocabas G.U., Gunlusoy B., Aydogdu O., Aydin M.E.: The relationship
between acquired premature ejaculation and metabolic syndrome: a prospective, comparative study. Int J Impot Res. 2017, 29 (3), 105–109. doi:
10.1038/ijir.2017.3. https://www.ncbi.nlm.nih.gov/pubmed/28179637
Borgdorff A.J., Bernabé J., Denys P., Alexandre L., Giuliano F.: Ejaculation elicited by microstimulation of lumbar spinothalamic neurons. Eur Urol. 2008,
54 (2), 449–456. doi: 10.1016/j.eururo.2008.03.043. https://www.ncbi.
nlm.nih.gov/pubmed/18394782
Brant W.O., Dean R.C., Lue T.F.: Treatment of Peyronie’s disease with oral
pentoxifylline. Nat Clin Pract Urol. 2006, 3 (2), 111–115. https://www.ncbi.
nlm.nih.gov/pubmed/16470210
Brant W.O., Garcia M.M., Bella A.J., Chi T., Lue T.F.: T-shaped shunt and intracavernous tunneling for prolonged ischemic priapism. J Urol. 2009, 181
(4), 1699–1705. doi: 10.1016/j.juro.2008.12.021. https://www.ncbi.nlm.
nih.gov/pubmed/19233430
Braun M., Wassmer G., Klotz T., Reifenrath B., Mathers M., Engelmann U.:
Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’.
Int J Impot Res. 2000, 12, 305–311. doi: 10.1038/sj.ijir.3900622. https://
www.ncbi.nlm.nih.gov/pubmed/11416833
Brock G., Nehra A., Lipshultz L.I., Karlin G.S., Gleave M., Seger M. i wsp.: Safety
and efficacy of vardenafil for the treatment of men with erectile dysfunction after radical retropubic prostatectomy. J Urol. 2003, 170, 1278–1283.
doi: 10.1097/01.ju.0000086947.00547.49. https://www.ncbi.nlm.nih.gov/
pubmed/14501741
Brock G., Ni X., Oelke M., Mulhall J., Rosenberg M., Seftel A. i wsp.: Efficacy
of Continuous Dosing of Tadalafil Once Daily vs Tadalafil On Demand
in Clinical Subgroups of Men With Erectile Dysfunction: A Descriptive
Comparison Using the Integrated Tadalafil Databases. J Sex Med. 2016,
13 (5), 860–875. doi: 10.1016/j.jsxm.2016.02.171. https://www.ncbi.nlm.
nih.gov/pubmed/27114197
Broderick G.A.: Priapism and sickle-cell anemia: diagnosis and nonsurgical therapy. J Sex Med. 2012, 9 (1), 88–103. doi: 10.1111/j.1743-
6109.2011.02317.x. https://www.ncbi.nlm.nih.gov/pubmed/21699659
Broderick G.A., Harkaway R.: Pharmacologic erection: time-dependent changes
in the corporal environment. Int J Impot Res. 1994, 6 (1), 9–16. https://
www.ncbi.nlm.nih.gov/pubmed/8019618
Broderick G.A., Kadioglu A., Bivalacqua T.J., Ghanem H., Nehra A., Shamloul
R.: Priapism: pathogenesis, epidemiology, and management. J Sex Med.
2010, 7, 476–500. doi: 10.1111/j.1743-6109.2009.01625.x. https://www.
ncbi.nlm.nih.gov/pubmed/20092449
Burnett A.L.: Fascia lata in penile reconstructive surgery: a reappraisal of
the fascia lata graft. Plast Reconstr Surg. 1997, 99 (4), 1061–1067. doi:
10.1097/00006534-199704000-00021. https://www.ncbi.nlm.nih.gov/
pubmed/9091903
Burnett A.L.: Surgical management of ischemic priapism. J Sex Med. 2012,
9 (1), 114–120. doi: 10.1111/j.1743-6109.2011.02446.x. https://www.ncbi.
nlm.nih.gov/pubmed/22221308
Burnett A.L., Allen R.P., Tempany C.M., Dover G.J., Brendler C.B.: Evaluation
of erectile function in men with sickle cell disease. Urology. 1995, 45 (4),
657–663. doi: 10.1016/s0090-4295(99)80059-4. https://www.ncbi.nlm.
nih.gov/pubmed/7716848
Burnett A.L., Bivalacwua T.J.: Priapism: new concepts in medical and surgical
management. Urol Clin North Am. 2011, 38 (2), 185–194. doi: 10.1016/j.
ucl.2011.02.005. https://www.ncbi.nlm.nih.gov/pubmed/21621085
Burnett A.L., Bivalacqua T.J., Champion H.C., Musicki B.: Feasibility of the
use of phosphodiesterase type 5 inhibitors in a pharmacologic prevention program for recurrent priapism. J Sex Med. 2006, 3 (6), 1077–1084.
doi: 10.1111/j.1743-6109.2006.00333.x. https://www.ncbi.nlm.nih.gov/
pubmed/17100941
Burnett A.L., Bivalacqua T.J., Champion H.C., Musicki B.: Long-term oral phosphodiesterase 5 inhibitor therapy alleviates recurrent priapism. Urology.
2006, 67 (5), 1043–1048. doi: 10.1016/j.urology.2005.11.045. https://www.
ncbi.nlm.nih.gov/pubmed/16698365
Burnett A.L., Pierorazio P.M.: Corporal “snake” maneuver: corporoglanular
shunt surgical modification for ischemic priapism. J Sex Med. 2009, 6 (4),
1171–1176. doi: 10.1111/j.1743-6109.2008.01176.x. https://www.ncbi.
nlm.nih.gov/pubmed/19207268
Burnett A.L., Sharlip I.D.: Standard operating procedures for priapism. J
Sex Med. 2013, 10 (1), 180–194. doi: 10.1111/j.1743-6109.2012.02707.x.
https://www.ncbi.nlm.nih.gov/pubmed/22462660
Burns P.R., Rosen R.C., Dunn M., Baygani S.K., Perelman M.A.: Treatment
satisfaction of men and partners following switch from on-demand phosphodiesterase type 5 inhibitor therapy to tadalafil 5mg once daily. J Sex
Med. 2015, 12 (3), 720–727. doi: 10.1111/jsm.12818. https://www.ncbi.
nlm.nih.gov/pubmed/25615445
Buvat J., Costa P., Morlier D., Lecocq B., Stegmann B., Albrecht D.: Double-blind
multicenter study comparing alprostadil alpha-cyclodextrin with moxisylyte chlorhydrate in patients with chronic erectile dysfunction. J Urol.
1998, 159 (1), 116–119. doi: 10.1016/s0022-5347(01)64030-8. https://
www.ncbi.nlm.nih.gov/pubmed/9400450
Buvat J., Hatzichristou D., Boess F.G., Büttner H., Gehchan N., Henneges C. i wsp.:
Continuation and effectiveness of tadalafil once daily during a 6-month
observational study in erectile dysfunction: the EDATE study. Int J Clin
Pract. 2014, 68 (9), 1087–1099. doi: 10.1111/ijcp.12449. https://www.ncbi.
nlm.nih.gov/pubmed/25123817
Buvat J., Maggi M., Gooren L., Guay A.T., Kaufman J., Morgentaler A. i wsp.:
Endocrine aspects of male sexual dysfunctions. J Sex Med. 2010, 7, 1627–
1656. doi: 10.1111/j.1743-6109.2010.01780.x. https://www.ncbi.nlm.nih.
gov/pubmed/20388162
Byers E.S., Grenier G.: Premature or rapid ejaculation: heterosexual couples’ perceptions of men’s ejaculatory behavior. Arch Sex Behav. 2003, 32
(3), 261–270. doi: 10.1023/a:1023417718557. https://www.ncbi.nlm.nih.
gov/pubmed/12807298
Cakan M., Altu Gcaron U., Aldemir M.: Is the combination of superselective transcatheter autologous clot embolization and duplex sonographyguided compression therapy useful treatment option for the patients with
high-flow priapism? Int J Impot Res. 2006, 18 (2), 141–145. doi: 10.1038/
sj.ijir.3901373. https://www.ncbi.nlm.nih.gov/pubmed/16079900
Calof O.M., Singh A.B., Lee M.L., Kenny A.M., Urban R.J., Tenover J.L. i wsp.:
Adverse events associated with testosterone replacement in middle-aged
and older men: a meta-analysis of randomized, placebo-controlled trials.
J Gerontol A Biol Sci Med Sci. 2005, 60 (11), 1451–1457. doi: 10.1093/
gerona/60.11.1451. https://www.ncbi.nlm.nih.gov/pubmed/16339333
Cantasdemir M., Gulsen F., Solak S., Numan F.: Posttraumatic high-flow priapism in children treated with autologous blood clot embolization: longterm results and review of the literature. Pediatr Radiol. 2011, 41 (6),
627–632. doi: 10.1007/s00247-010-1912-3. https://www.ncbi.nlm.nih.
gov/pubmed/21127852
Capogrosso P., Colicchia M., Ventimiglia E., Castagna G., Clementi M.C., Suardi
N. i wsp.: One patient out of four with newly diagnosed erectile dysfunction
is a young man--worrisome picture from the everyday clinical practice. J
Sex Med. 2013, 10 (7), 1833–1841. doi: 10.1111/jsm.12179. https://www.
ncbi.nlm.nih.gov/pubmed/23651423
Capogrosso P., Ventimiglia E., Boeri L., Serino A., Russo A., La Croce G. i wsp.:
Time of onset of vardenafil orodispersible tablet in a real-life setting - looking beyond randomized clinical trials. Expert Rev Clin Pharmacol. 2017,
10 (3), 339–344. doi: 10.1080/17512433.2017.1288567. https://www.ncbi.
nlm.nih.gov/pubmed/28129714
Carani C., Isidori A.M., Granata A., Carosa E., Maggi M., Lenzi A. i wsp.:
Multicenter study on the prevalence of sexual symptoms in male hypoand hyperthyroid patients. J Clin Endocrinol Metab. 2005, 90 (12),
6472–6479. doi: 10.1210/jc.2005-1135. https://www.ncbi.nlm.nih.gov/
pubmed/16204360
Caretta N., de Kreutzenberg S.V., Valente U., Guarneri G., Ferlin A., Avogaro A.
i wsp.: Hypovitaminosis D is associated with erectile dysfunction in type
2 diabetes. Endocrine. 2016, 53 (3), 831–838. doi: 10.1007/s12020-015-
0851-z. https://www.ncbi.nlm.nih.gov/pubmed/26758995
Carrieri M.P., Serraino D., Palmiotto F., Nucci G., Sasso F.: A case-control study
on risk factors for Peyronie’s disease. J Clin Epidemiol, 1998, 51 (6), 511–
515. doi: 10.1016/s0895-4356(98)00015-8. https://www.ncbi.nlm.nih.
gov/pubmed/9636000
Carson C.C.: Penile prosthesis implantation in the treatment of Peyronie’s
disease. Int J Impot Res. 1998, 10 (2), 125–128. doi: 10.1038/sj.ijir.3900330.
https://www.ncbi.nlm.nih.gov/pubmed/9647951
Carson C., Gunn K.: Premature ejaculation: definition and prevalence. Int J
Impot Res. 2006, 18 Suppl 1, S5–13. doi: 10.1038/sj.ijir.3901507. https://
www.ncbi.nlm.nih.gov/pubmed/16953247
Carson C.C., Mulcahy J.J., Govier F.E.: Efficacy, safety and patient satisfaction outcomes of the AMS 700CX inflatable penile prosthesis: results of a
long-term multicenter study. AMS 700CX Study Group. J Urol. 2000, 164
(2), 376–380. https://www.ncbi.nlm.nih.gov/pubmed/10893589
Carson C.C., Mulcahy J.J., Harsch M.R.: Long-term infection outcomes after
original antibiotic impregnated inflatable penile prosthesis implants: up
to 7.7 years of followup. J Urol. 2011, 185 (2), 614–618. doi: 10.1016/j.
juro.2010.09.094. https://www.ncbi.nlm.nih.gov/pubmed/21168870
Carson C.C., Sadeghi-Nejad H., Tursi J.P., Smith T.M., Kaufman G.J., Gilbert
K. i wsp.: Analysis of the clinical safety of intralesional injection of collagenase Clostridium histolyticum (CCH) for adults with Peyronie’s disease
(PD). BJU Int. 2015, 116 (5), 815–822. doi: 10.1111/bju.13120. https://
www.ncbi.nlm.nih.gov/pubmed/25818264
Casabe A.R., Sarotto N., Gutierrez C., Bechara A.J.: Satisfaction assessment
with malleable prosthetic implant of Spectra (AMS) and Genesis (Coloplast)
models. Int J Impot Res. 2016, 28 (6), 228–233. doi: 10.1038/ijir.2016.33.
https://www.ncbi.nlm.nih.gov/pubmed/27557609
Castiglione F., Albersen M., Hedlund P., Gratzke C., Salonia A., Giuliano F.: Current
Pharmacological Management of Premature Ejaculation: A Systematic
Review and Meta-analysis. Eur Urol. 2016, 69 (5), 904–916. doi: 10.1016/j.
eururo.2015.12.028. https://www.ncbi.nlm.nih.gov/pubmed/26749092
Cavallini G.: Resolution of erectile dysfunction after an andrological visit in a
selected population of patients affected by psychogenic erectile dysfunction.
Asian J Androl. 2017, 19 (2), 219–222. doi: 10.4103/1008-682X.172646.
https://www.ncbi.nlm.nih.gov/pubmed/26806083
Cavallini G., Biagiotti G., Koverech A., Vitali G.: Oral propionyl-l-carnitine and intraplaque verapamil in the therapy of advanced and resistant
Peyronie’s disease. BJU Int. 2002, 89 (9), 895–900. doi: 10.1046/j.1464-
410x.2002.02738.x. https://www.ncbi.nlm.nih.gov/pubmed/12010235
Cavallini G., Modenini F., Vitali G.: Open preliminary randomized prospective clinical trial of efficacy and safety of three different verapamil dilutions for intraplaque therapy of Peyronie’s disease. Urology. 2007, 69 (5),
950–954. doi: 10.1016/j.urology.2007.01.080. https://www.ncbi.nlm.nih.
gov/pubmed/17482941
Champion H.C., Bivalacqua T.J., Takimoto E., Kass D.A., Burnett A.L.:
Phosphodiesterase-5A dysregulation in penile erectile tissue is a mechanism
of priapism. Proc Natl Acad Sci U S A. 2005, 102 (5), 1661–1666. doi: 10.1073/
pnas.0407183102. https://www.ncbi.nlm.nih.gov/pubmed/15668387
Chaudhary M., Sheikh N., Asterling S., Ahmad I., Greene D.: Peyronie’s disease
with erectile dysfunction: penile modeling over inflatable penile prostheses. Urology. 2005, 65 (4), 760–764. doi: 10.1016/j.urology.2004.10.039.
https://www.ncbi.nlm.nih.gov/pubmed/15833523
Chen J., Mabjeesh N.J., Matzkin H., Greenstein A.: Efficacy of sildenafil as
adjuvant therapy to selective serotonin reuptake inhibitor in alleviating
premature ejaculation. Urology. 2003, 61 (1), 197–200. doi: 10.1016/s0090-
4295(02)02075-7. https://www.ncbi.nlm.nih.gov/pubmed/12559295
Chen L., Staubli S.E., Schneider M.P., Kessels A.G., Ivic S., Bachmann L.M.
i wsp.: Phosphodiesterase 5 inhibitors for the treatment of erectile dysfunction: A trade-off network meta-analysis. Eur Urol. 2015, 68 (4), 674–
680. doi: 10.1016/j.eururo.2015.03.031. https://www.ncbi.nlm.nih.gov/
pubmed/25817916
Chen Y.F., Lin H.H., Lu C.C., Hung C.T., Lee M.H., Hsu C.Y.: Gout and a
Subsequent Increased Risk of Erectile Dysfunction in Men Aged 64 and
Under: A Nationwide Cohort Study in Taiwan. J Rheumatol. 2015, 42 (10),
1898–1905. doi: 10.3899/jrheum.141105. https://www.ncbi.nlm.nih.gov/
pubmed/26077405
Christodoulidou M., Pearce I.: Infection of Penile Prostheses in Patients with
Diabetes Mellitus. Surg Infect (Larchmt). 2016, 17 (1), 2–8. doi: 10.1089/
sur.2015.164. https://www.ncbi.nlm.nih.gov/pubmed/26426099
Chun J.L., McGregor A., Krishnan R., Carson C.C.: A comparison of dermal
and cadaveric pericardial grafts in the modified Horton-Devine procedure
for Peyronie’s disease. J Urol. 2001, 166 (1), 185–188. https://www.ncbi.
nlm.nih.gov/pubmed/11435853
Chung E., Broc G.B.: A state of art review on vardenafil in men with erectile
dysfunction and associated underlying diseases. Expert Opin Pharmacother.
2011, 12 (8), 1341–1348. doi: 10.1517/14656566.2011.584064. https://
www.ncbi.nlm.nih.gov/pubmed/21548725
Chung E., Cartmill R.: Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the
treatment of male erectile dysfunction: an Australian first open-label single-arm prospective clinical trial. BJU Int. 2015, 5, 46–49. doi: 10.1111/
bju.13035. https://www.ncbi.nlm.nih.gov/pubmed/25828173
Chung E., Deyoung L., Brock G.B.: The role of PDE5 inhibitors in penile septal scar remodeling: assessment of clinical and radiological outcomes. J
Sex Med. 2011, 8 (5), 1472–1477. doi: 10.1111/j.1743-6109.2011.02217.x.
https://www.ncbi.nlm.nih.gov/pubmed/21324095
Chung E., Van C.T., Wilson I., Cartmill R.A.: Penile prosthesis implantation for
the treatment for male erectile dysfunction: clinical outcomes and lessons
learnt after 955 procedures. World J Urol. 2013, 31 (3), 591–595. doi: 10.1007/
s00345-012-0859-4. https://www.ncbi.nlm.nih.gov/pubmed/22457032
Cipollone G., Nicolai M., Mastroprimiano G., Iantorno R., Longeri D., Tenaglia R.:
[Betamethasone versus placebo in Peyronie’s disease]. Arch Ital Urol Androl.
1998, 70 (4), 165–168. https://www.ncbi.nlm.nih.gov/pubmed/9823662
Clavijo R.I., Kohn T.P., Kohn J.R., Ramasamy R.: Effects of Low-Intensity
Extracorporeal Shockwave Therapy on Erectile Dysfunction: A Systematic
Review and Meta-Analysis. J Sex Med. 2017, 14 (1), 27–35. doi: 10.1016/j.
jsxm.2016.11.001. https://www.ncbi.nlm.nih.gov/pubmed/27986492
Cookson M.S., Nadig P.W.: Long-term results with vacuum constriction device.
J Urol. 1993, 149 (2), 290–294. doi: 10.1016/s0022-5347(17)36059-7. https://
www.ncbi.nlm.nih.gov/pubmed/8426404
Coombs P.G., Heck M., Guhring P., Narus J., Mulhall J.P.: A review of outcomes
of an intracavernosal injection therapy programme. BJU Int. 2012, 110
(11), 1787–1791. doi: 10.1111/j.1464-410X.2012.11080.x. https://www.
ncbi.nlm.nih.gov/pubmed/22564343
Cooper K., Martyn-St James M., Kaltenthaler E., Dickinson K., Cantrell A., Wylie
K. i wsp.: Behavioral Therapies for Management of Premature Ejaculation:
A Systematic Review. Sex Med. 2015, 3 (3), 174–188. doi: 10.1002/sm2.65.
https://www.ncbi.nlm.nih.gov/pubmed/26468381
Corbetta J.P., Durán V., Burek C., Sager C., Weller S., Paz E. i wsp.: High flow
priapism: diagnosis and treatment in pediatric population. Pediatr Surg
Int. 2011, 27 (11), 1217–1221. doi: 10.1007/s00383-011-2911-7. https://
www.ncbi.nlm.nih.gov/pubmed/21544645
Cordeiro E.R., Cathelineau X., Thüroff S., Marberger M., Crouzet S., de la Rosette
J.J.: High-intensity focused ultrasound (HIFU) for definitive treatment of
prostate cancer. BJU Int. 2012, 110 (9), 1228–1242. doi: 10.1111/j.1464-
410X.2012.11262.x. https://www.ncbi.nlm.nih.gov/pubmed/22672199
Cormio L., Massenio P., La Rocca R., Verze P., Mirone V., Carrieri G.: The
Combination of Dapoxetine and Behavioral Treatment Provides Better
Results than Dapoxetine Alone in the Management of Patients with Lifelong
Premature Ejaculation. J Sex Med. 2015, 12 (7), 1609–1615. doi: 10.1111/
jsm.12925. https://www.ncbi.nlm.nih.gov/pubmed/26077706
Cormio L., Zucchi A., Lorusso F., Selvaggio O., Fioretti F., Porena M. i wsp.:
Surgical treatment of Peyronie’s disease by plaque incision and grafting
with buccal mucosa. Eur Urol. 2009, 55 (6), 1469–1475. doi: 10.1016/j.
eururo.2008.11.041. https://www.ncbi.nlm.nih.gov/pubmed/19084325
Corona G., Maseroli E., Rastrelli G., Isidori A.M., Sforza A., Mannucci E. i wsp.:
Cardiovascular risk associated with testosterone-boosting medications: a
systematic review and meta-analysis. Expert Opin Drug Saf. 2014, 13 (10),
1327–1351. doi: 10.1517/14740338.2014.950653. https://www.ncbi.nlm.
nih.gov/pubmed/25139126
Corona G., Rastrelli G., Burri A., Jannini E.A., Maggi M.: The safety and efficacy of Avanafil, a new 2nd generation PDE5i: Comprehensive review
and meta-analysis. Expert Opin Drug Saf. 2016, 15 (2), 237–247. doi:
10.1517/14740338.2016.1130126. https://www.ncbi.nlm.nih.gov/
pubmed/26646748
Corona G., Rastrelli G., Burri A., Serra E., Gianfrilli D., Mannucci E. i wsp.: Firstgeneration phosphodiesterase type 5 inhibitors dropout: a comprehensive
review and meta-analysis. Andrology. 2016, 4 (6), 1002–1009. doi: 10.1111/
andr.12255. https://www.ncbi.nlm.nih.gov/pubmed/27636710
Corona G., Rastrelli G., Limoncin E., Sforza A., Jannini E.A., Maggi M. i wsp.:
Interplay Between Premature Ejaculation and Erectile Dysfunction: A
Systematic Review and Meta-Analysis. J Sex Med. 2015, 12 (12), 2291–2300.
doi: 10.1111/jsm.13041. https://www.ncbi.nlm.nih.gov/pubmed/26552599
Costa P., Potempa A.J.: Intraurethral alprostadil for erectile dysfunction: a review of the literature. Drugs. 2012, 72 (17), 2243–2254. doi:
10.2165/11641380-000000000-00000. https://www.ncbi.nlm.nih.gov/
pubmed/23170913
Cui H., Liu B., Song Z., Fang J., Deng Y., Zhang S. i wsp.: Efficacy and safety
of long-term tadalafil 5 mg once daily combined with sildenafil 50 mg as
needed at the early stage of treatment for patients with erectile dysfunction. Andrologia. 2015, 47 (1), 20–24. doi: 10.1111/and.12216. https://
www.ncbi.nlm.nih.gov/pubmed/24387078
Curran M., Keating G.: Tadalafil. Drugs. 2003, 63 (20), 2203–2212. doi:
10.2165/00003495-200363200-00004. https://www.ncbi.nlm.nih.gov/
pubmed/14498756
D’Aleo G., Rifici C., Kofler M., Saltuari L., Bramanti P.: Favorable response
to intrathecal, but not oral, baclofen of priapism in a patient with spinal
cord injury. Spine (Phila Pa 1976). 2009, 34 (3), E127–129. doi: 10.1097/
BRS.0b013e31818d04ff. https://www.ncbi.nlm.nih.gov/pubmed/19179913
Dalkin B.L., Carter M.F.: Venogenic impotence following dermal graft repair
for Peyronie’s disease. J Urol. 1991, 146 (3), 849–851. doi: 10.1016/s0022-
5347(17)37941-7. https://www.ncbi.nlm.nih.gov/pubmed/1843616
Daoud A.S., Bataineh H., Otoom S., Abdul-Zahra E.: The effect of Vigabatrin,
Lamotrigine and Gabapentin on the fertility, weights, sex hormones and
biochemical profiles of male rats. Neuro Endocrinol Lett. 2004, 25 (3), 178–
183. https://www.ncbi.nlm.nih.gov/pubmed/15349082
Darouiche R.O., Bella A.J., Boone T.B., Brock G., Broderick G.A., Burnett A.L.
i wsp.: North American consensus document on infection of penile prostheses. Urology. 2013, 82 (4), 937–942. doi: 10.1016/j.urology.2013.05.048.
https://www.ncbi.nlm.nih.gov/pubmed/23958508
Das S.: Peyronie’s disease: excision and autografting with tunica vaginalis. J
Urol. 1980, 124 (6), 818–819. doi: 10.1016/s0022-5347(17)55682-7. https://
www.ncbi.nlm.nih.gov/pubmed/7441830
Datta N.S.: Megalophallus in sickle cell disease. J Urol. 1977, 117 (5), 672–
673. doi: 10.1016/s0022-5347(17)58582-1. https://www.ncbi.nlm.nih.gov/
pubmed/859210
Davila H.H., Parker J., Webster J.C., Lockhart J.L., Carrion R.E.: Subarachnoid
hemorrhage as complication of phenylephrine injection for the treatment
of ischemic priapism in a sickle cell disease patient. J Sex Med. 2008, 5 (4),
1025–1028. doi: 10.1111/j.1743-6109.2007.00715.x. https://www.ncbi.
nlm.nih.gov/pubmed/18194188
Davis-Joseph B., Tiefer L., Melman A.: Accuracy of the initial history and physical examination to establish the etiology of erectile dysfunction. Urology.
1995, 45 (3), 498–502. doi: 10.1016/s0090-4295(99)80022-3. https://www.
ncbi.nlm.nih.gov/pubmed/7879338
De Amicis L.A., Goldberg D.C., LoPiccolo J., Friedman J., Davies L.: Clinical
follow-up of couples treated for sexual dysfunction. Arch Sex Behav. 1985,
14 (6), 467–489. doi: 10.1007/bf01541749. https://www.ncbi.nlm.nih.gov/
pubmed/4084048
de Carufel F., Trudel G.: Effects of a new functional-sexological treatment for premature ejaculation. J Sex Marital Ther. 2006, 32 (2), 97–114.
doi: 10.1080/00926230500442292. https://www.ncbi.nlm.nih.gov/
pubmed/16418103
Debruyne F.M., Gittelman M., Sperling H., Börner M., Beneke M.: Time to onset
of action of vardenafil: a retrospective analysis of the pivotal trials for the
orodispersible and film-coated tablet formulations. J Sex Med. 2011, 8
(10), 2912–2923. doi: 10.1111/j.1743-6109.2011.02462.x. https://www.
ncbi.nlm.nih.gov/pubmed/21883954
DeBusk R., Drory Y., Goldstein I., Jackson G., Kaul S., Kimmel S.E. i wsp.:
Management of sexual dysfunction in patients with cardiovascular disease: recommendations of The Princeton Consensus Panel. Am J Cardiol.
2000, 86 (2), 175–181. doi: 10.1016/s0002-9149(00)00896-1. https://www.
ncbi.nlm.nih.gov/pubmed/10913479
DeCastro B.J., Costabile R.A., McMann L.P., Peterson A.C.: Oral ketoconazole
for prevention of postoperative penile erection: a placebo controlled, randomized, double-blind trial. J Urol. 2008, 179 (5), 1930–1932. doi: 10.1016/j.
juro.2008.01.039. https://www.ncbi.nlm.nih.gov/pubmed/18353393
Desanctis P.N., Furey C.A.: Steroid injection therapy for Peyronie’s disease:
a 10-year summary and review of 38 cases. J Urol. 1967, 97 (1), 114–116.
doi: 10.1016/s0022-5347(17)62993-8. https://www.ncbi.nlm.nih.gov/
pubmed/6016195
Deveci S., Hopps C.V., O’Brien K., Parker M., Guhring P., Mulhall J.P.: Defining
the clinical characteristics of Peyronie’s disease in young men. J Sex Med.
2007, 4 (2), 485–490. doi: 10.1111/j.1743-6109.2006.00344.x. https://
www.ncbi.nlm.nih.gov/pubmed/17081219
Devine C.J., Horton C.E.: Surgical treatment of Peyronie’s disease with a dermal graff. J Urol. 1974, 111 (1), 44–49. doi: 10.1016/s0022-5347(17)59886-
9. https://www.ncbi.nlm.nih.gov/pubmed/4273261
Devine C.J., Somers K.D., Jordan S.G., Schlossberg S.M.: Proposal: trauma as the
cause of the Peyronie’s lesion. J Urol. 1997, 157 (1), 285–290. doi: 10.1016/
s0022-5347(01)65361-8. https://www.ncbi.nlm.nih.gov/pubmed/8976281
Di Stasi S.M., Giannantoni A., Capelli G., Jannini E.A., Virgili G., Storti L. i wsp.:
Transdermal electromotive administration of verapamil and dexamethasone
for Peyronie’s disease. BJU Int. 2003, 91 (9), 825–829. doi: 10.1046/j.1464-
410x.2003.04242.x. https://www.ncbi.nlm.nih.gov/pubmed/12780842
Dinsmore W.W., Wyllie M.G.: Vasoactive intestinal polypeptide/phentolamine for intracavernosal injection in erectile dysfunction. BJU Int. 2008,
102 (8), 933–937. doi: 10.1111/j.1464-410X.2008.07764.x. https://www.
ncbi.nlm.nih.gov/pubmed/18485029
Dong J.Y., Zhang Y.H., Qin L.Q.: Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J Am Coll Cardiol.
2011, 58 (13), 1378–1385. doi: 10.1016/j.jacc.2011.06.024. https://www.
ncbi.nlm.nih.gov/pubmed/21920268
DSM, V., American Psychiatric Association. Diagnostic and Statistical Manual
of Mental Disorders, Fifth Edition. 2013, Arlington, VA. http://www.dsm5.
org/psychiatrists/practice/dsm
Dubocq F.M., Tefilli M.V., Grignon D.J., Pontes J.E., Dhabuwala C.B.: High
flow malignant priapism with isolated metastasis to the corpora cavernosa. Urology. 1998, 51 (2), 324–326. doi: 10.1016/s0090-4295(97)00607-
9. https://www.ncbi.nlm.nih.gov/pubmed/9495721
Duman D.G., Biçakci E., Çelikel Ç.A., Akbal C.: Nonalcoholic Fatty Liver Disease
is Associated with Erectile Dysfunction: A Prospective Pilot Study. J Sex
Med. 2016, 13 (3), 383–388. doi: 10.1016/j.jsxm.2015.12.030. https://www.
ncbi.nlm.nih.gov/pubmed/26853046
Duncan M.R., Berman B., Nseyo U.O.: Regulation of the proliferation and
biosynthetic activities of cultured human Peyronie’s disease fibroblasts
by interferons-alpha, -beta and -gamma. Scand J Urol Nephrol. 1991, 25
(2), 89–94. doi: 10.3109/00365599109024539. https://www.ncbi.nlm.nih.
gov/pubmed/1651559
Dunn K.M., Croft P.R., Hackett G.I.: Association of sexual problems with
social, psychological, and physical problems in men and women: a cross
sectional population survey. J Epidemiol Community Health. 1999, 53
(3), 144–148. doi: 10.1136/jech.53.3.144. https://www.ncbi.nlm.nih.gov/
pubmed/10396490
Eardley I., Donatucci C., Corbin J., El-Meliegy A., Hatzimouratidis K., McVary
K. i wsp.: Pharmacotherapy for erectile dysfunction. J Sex Med. 2010, 7,
524–540. doi: 10.1111/j.1743-6109.2009.01627.x. https://www.ncbi.nlm.
nih.gov/pubmed/20092451
Eardley I., Montorsi F., Jackson G., Mirone V., Chan M.L., Loughney K. i wsp.:
Factors associated with preference for sildenafil citrate and tadalafil for
treating erectile dysfunction in men naive to phosphodiesterase 5 inhibitor
therapy: post hoc analysis of data from a multicentre, randomized, openlabel, crossover study. BJU Int. 2007, 100 (1), 122–129. doi: 10.1111/j.1464-
410X.2007.06916.x. https://www.ncbi.nlm.nih.gov/pubmed/17552960
Ebbehoj J.: A new operation for priapism. Scand J Plast Reconstr Surg. 1974,
8 (3), 241–242. doi: 10.3109/02844317409084400. https://www.ncbi.nlm.
nih.gov/pubmed/4458048
Ebbehoj J., Metz P.: Congenital penile angulation. Br J Urol. 1987, 60 (3),
264–266. doi: 10.1111/j.1464-410x.1987.tb05497.x. https://www.ncbi.
nlm.nih.gov/pubmed/3676675
Ebbehoj J., Metz P.: New operation for “krummerik” (penile curvature).
Urology. 1985, 26 (1), 76–78. doi: 10.1016/0090-4295(85)90264-x. https://
www.ncbi.nlm.nih.gov/pubmed/3892851
Egeberg A., Hansen P.R., Gislason G.H., Skov L., Thyssen J.P.: Erectile dysfunction in male adults with atopic dermatitis and psoriasis. J Sex Med. 2017,
14 (3), 380–386. doi: 10.1016/j.jsxm.2016.12.233. https://www.ncbi.nlm.
nih.gov/pubmed/28109691
Egydio P.H., Lucon A.M., Arap S.: A single relaxing incision to correct different
types of penile curvature: surgical technique based on geometrical principles.
BJU Int. 2004, 94 (7), 1147–1157. doi: 10.1111/j.1464-410X.2004.05220.x.
https://www.ncbi.nlm.nih.gov/pubmed/15541152
Ehrlich H.P.: Scar contracture: cellular and connective tissue aspects in
Peyronie’s disease. J Urol. 1997, 157 (1), 316–319. doi: 10.1016/s0022-
5347(01)65368-0. https://www.ncbi.nlm.nih.gov/pubmed/8976288
Eland I.A., van der Lei J., Stricker B.H., Sturkenboom M.J.: Incidence of priapism
in the general population. Urology. 2001, 57 (5), 970–972. doi: 10.1016/
s0090-4295(01)00941-4. https://www.ncbi.nlm.nih.gov/pubmed/11337305
El-Bahnasawy M.S., Dawood A., Farouk A.: Low-flow priapism: risk factors for
erectile dysfunction. BJU Int. 2002, 89 (3), 285–290. doi: 10.1046/j.1464-
4096.2001.01510.x. https://www.ncbi.nlm.nih.gov/pubmed/11856112
El-Nashaar A., Shamlout R.: Antibiotic treatment can delay ejaculation in
patients with premature ejaculation and chronic bacterial prostatitis. J
Sex Med. 2007, 4 (2), 491–496. doi: 10.1111/j.1743-6109.2006.00243.x.
https://www.ncbi.nlm.nih.gov/pubmed/17367444
El-Sakka A.I., Rashwan H.M., Lue T.F.: Venous patch graft for Peyronie’s
disease. Part II: outcome analysis. J Urol. 1998, 162, 2050–2053. doi:
10.1097/00005392-199812010-00030. https://www.ncbi.nlm.nih.gov/
pubmed/9817321
EMA. Assessement Report - Xiapex (Collagenase Clostridium Histolyticum).
2014. https://www.ema.europa.eu/documents/assessment-report/
xiapex-epar-public-assessment-report_en.pdf
Emond A.M., Holman R., Hayes R.J., Serjeant G.R.: Priapism and impotence
in homozygous sickle cell disease. Arch Intern Med. 1980, 140 (11), 1434–
1437. https://www.ncbi.nlm.nih.gov/pubmed/6159833
Eracleous E., Kondou M., Aristidou K., Eliades S., Pantziaris M., Posporis T.: Use
of Doppler ultrasound and 3-dimensional contrast-enhanced MR angiography in the diagnosis and follow-up of post-traumatic high-flow priapism in a
child. Pediatr Radiol. 2000, 30 (4), 265–267. doi: 10.1007/s002470050736.
https://www.ncbi.nlm.nih.gov/pubmed/10789908
Ercole C.J., Pontes J.E., Pierce J.M.: Changing surgical concepts in the
treatment of priapism. J Urol. 1981, 125 (2), 210–211. doi: 10.1016/
s0022-5347(17)54971-x. https://www.ncbi.nlm.nih.gov/pubmed/7206057
Essed E., Schroeder F.H.: New surgical treatment for Peyronie disease. Urology.
1985, 25 (6), 582–587. doi: 10.1016/0090-4295(85)90285-7. https://www.
ncbi.nlm.nih.gov/pubmed/4012950
Faerber G.J., Konnak J.W.: Results of combined Nesbit penile plication with
plaque incision and placement of Dacron patch in patients with severe
Peyronie’s disease. J Urol. 1993, 149, 1319–1320. https://www.ncbi.nlm.
nih.gov/pubmed/8479026
Falcone M., Rolle L., Ceruti C., Timpano M., Sedigh O., Preto M. i wsp.: Prospective
analysis of the surgical outcomes and patients’ satisfaction rate after the
AMS Spectra penile prosthesis implantation. Urology. 2013, 82 (2), 373–
376. doi: 10.1016/j.urology.2013.04.027. https://www.ncbi.nlm.nih.gov/
pubmed/23791218
Fallon B.: Cadaveric dura mater graft for correction of penile curvature
in Peyronie disease. Urology. 1990, 35 (2), 127–129. doi: 10.1016/0090-
4295(90)80058-u. https://www.ncbi.nlm.nih.gov/pubmed/2305535
Fan D., Liu L., Ding N., Liu S., Hu Y., Cai G. i wsp.: Male sexual dysfunction and ankylosing spondylitis: a systematic review and metaanalysis. J
Rheumatol. 2015, 42 (2), 252–257. doi: 10.3899/jrheum.140416. https://
www.ncbi.nlm.nih.gov/pubmed/25448789
Fang S.C., Rosen R.C., Vita J.A., Ganz P., Kupelian V.: Changes in erectile
dysfunction over time in relation to Framingham cardiovascular risk in
the Boston Area Community Health (BACH) Survey. J Sex Med. 2015, 12
(1), 100–108. doi: 10.1111/jsm.12715. https://www.ncbi.nlm.nih.gov/
pubmed/25293632
Farag Y.M., Guallar E., Zhao D., Kalyani R.R., Blaha M.J., Feldman D.I. i wsp.:
Vitamin D deficiency is independently associated with greater prevalence
of erectile dysfunction: The National Health and Nutrition Examination
Survey (NHANES) 2001–2004. Atherosclerosis. 2016, 252, 61–67. doi:
10.1016/j.atherosclerosis.2016.07.921. https://www.ncbi.nlm.nih.gov/
pubmed/27505344
FDA, U. Warning letter to William Weldon, CEO & Chairman of Johnson
& Johnson, regarding Ultram-ER web advertisement. 2009.
Feldman H.A., Goldstein I., Hatzichristou D.G., Krane R.J., McKinlay J.B.:
Impotence and its medical and psychosocial correlates: results of the
Massachusetts Male Aging Study. J Urol. 1994, 151 (1), 54–61. doi: 10.1016/
s0022-5347(17)34871-1. https://www.ncbi.nlm.nih.gov/pubmed/8254833
Fernandez-Balsells M.M., Murad M.H., Lane M., Lampropulos J.F., Albuquerque
F., Mullan R.J. i wsp.: Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol
Metab. 2010, 95 (6), 2560–2575. doi: 10.1210/jc.2009-2575. https://www.
ncbi.nlm.nih.gov/pubmed/20525906
Ferrini M.G., Davila H.H., Kovanecz I., Sanchez S.P., Gonzalez-Cadavid N.F.,
Rajfer J.: Vardenafil prevents fibrosis and loss of corporal smooth muscle
that occurs after bilateral cavernosal nerve resection in the rat. Urology.
2006, 68 (2), 429–435. doi: 10.1016/j.urology.2006.05.011. https://www.
ncbi.nlm.nih.gov/pubmed/16904479
Ferrini M.G., Kovanecz I., Nolazco G., Rajfer J., Gonzalez-Cadavid N.F.: Effects
of long-term vardenafil treatment on the development of fibrotic plaques
in a rat model of Peyronie’s disease. BJU Int. 2006, 97 (3), 625–633. doi:
10.1111/j.1464-410X.2006.05955.x. https://www.ncbi.nlm.nih.gov/
pubmed/16469038
Ferrini M.G., Kovanecz I., Sanchez S., Vernet D., Davila H.H., Rajfer J. i wsp.:
Long-term continuous treatment with sildenafil ameliorates aging-related
erectile dysfunction and the underlying corporal fibrosis in the rat. Biol
Reprod. 2007, 76 (5), 915–923. doi: 10.1095/biolreprod.106.059642. https://
www.ncbi.nlm.nih.gov/pubmed/17287493
Ficarra V., Novara G., Ahlering T.E., Costello A., Eastham J.A., Graefen M. i wsp.:
Systematic review and meta-analysis of studies reporting potency rates
after robot-assisted radical prostatectomy. Eur Urol. 2012, 62 (3), 418–
420. doi: 10.1016/j.eururo.2012.05.046. https://www.ncbi.nlm.nih.gov/
pubmed/22749850
Fisher W.A., Eardley I., McCabe M., Sand M.: Erectile dysfunction (ED) is a
shared sexual concern of couples I: couple conceptions of ED. J Sex Med.
2009, 6, 2746–2760. doi: 10.1111/j.1743-6109.2009.01457.x. https://www.
ncbi.nlm.nih.gov/pubmed/19694926
Fojecki G.L., Tiessen S., Osther P.J.: Effect of Low-Energy Linear Shockwave
Therapy on Erectile Dysfunction – A Double-Blinded, Sham-Controlled,
Randomized Clinical Trial. J Sex Med. 2017, 14 (1), 106–112. doi: 10.1016/j.
jsxm.2016.11.307. https://www.ncbi.nlm.nih.gov/pubmed/27938990
Forgue S.T., Patterson B.E., Bedding A.W., Payne C.D., Phillips D.L., Wrishko R.E.
i wsp.: Tadalafil pharmacokinetics in healthy subjects. Br J Clin Pharmacol.
2006, 61 (3), 280–288. doi: 10.1111/j.1365-2125.2005.02553.x. https://
www.ncbi.nlm.nih.gov/pubmed/16487221
Fowler J.E., Koshy M., Strub M., Chinn S.K.: Priapism associated with the
sickle cell hemoglobinopathies: prevalence, natural history and sequelae. J
Urol. 1991, 145 (1), 65–68. doi: 10.1016/s0022-5347(17)38248-4. https://
www.ncbi.nlm.nih.gov/pubmed/1984102
Frink M.C., Hennies H.H., Englberger W., Haurand M., Wilffert B.:
Influence of tramadol on neurotransmitter systems of the rat brain.
Arzneimittelforschung. 1996, 46 (11), 1029–1036. https://www.ncbi.nlm.
nih.gov/pubmed/8955860
Furtado P.S., Costa M.P., Ribeiro do Prado Valladares F., Oliveira da Silva L.,
Lordêlo M., Lyra I. i wsp.: The prevalence of priapism in children and adolescents with sickle cell disease in Brazil. Int J Hematol. 2012, 95 (6), 648–
651. doi: 10.1007/s12185-012-1083-0. https://www.ncbi.nlm.nih.gov/
pubmed/22539365
Gacci M., Andersson K.E., Chapple C., Maggi M., Mirone V., Oelke M. i wsp.:
Latest Evidence on the Use of Phosphodiesterase Type 5 Inhibitors for
the Treatment of Lower Urinary Tract Symptoms Secondary to Benign
Prostatic Hyperplasia. Eur Urol. 2016, 70 (1), 124–133. doi: 10.1016/j.
eururo.2015.12.048. https://www.ncbi.nlm.nih.gov/pubmed/26806655
Gandaglia G., Briganti A., Jackson G., Kloner R.A., Montorsi F., Montorsi P.
i wsp.: A systematic review of the association between erectile dysfunction
and cardiovascular disease. Eur Urol. 2014, 65 (5), 968–978. doi: 10.1016/j.
eururo.2013.08.023. https://www.ncbi.nlm.nih.gov/pubmed/24011423
Garaffa G., Sacca A., Christopher A.N., Ralph D.J.: Circumcision is not mandatory in penile surgery. BJU Int. 2010, 105 (2), 222–224. doi: 10.1111/j.1464-
410X.2009.08763.x. https://www.ncbi.nlm.nih.gov/pubmed/19594732
Garcia-Gomez B., Ralph D., Levine L., Moncada-Iribarren I., Djinovic R., Albersen
M. i wsp.: Grafts for Peyronie’s disease: a comprehensive review. Andrology.
2018, 6 (1), 117–126. doi: 10.1111/andr.12421. https://www.ncbi.nlm.nih.
gov/pubmed/29266877
Gazzaruso C., Coppola A., Montalcini T., Valenti C., Garzaniti A., Pelissero G.
i wsp.: Erectile dysfunction can improve the effectiveness of the current
guidelines for the screening for asymptomatic coronary artery disease in
diabetes. Endocrine. 2011, 40 (2), 273–279. doi: 10.1007/s12020-011-9523-
9. https://www.ncbi.nlm.nih.gov/pubmed/21861245
Gbadoe A.D., Atakouma Y., Kusiaku K., Assimadi J.K.: Management of sickle cell
priapism with etilefrine. Arch Dis Child. 2001, 85 (1), 52–53. doi: 10.1136/
adc.85.1.52. https://www.ncbi.nlm.nih.gov/pubmed/11420201
Gelbard M.K., Dorey F., James K.: The natural history of Peyronie’s disease.
J Urol. 1990, 144 (6), 1376–1379. doi: 10.1016/s0022-5347(17)39746-x.
https://www.ncbi.nlm.nih.gov/pubmed/2231932
Gelbard M.K., Hayden B.: Expanding contractures of the tunica albuginea
due to Peyronie’s disease with temporalis fascia free grafts. J Urol. 1991,
145 (4), 772–776. doi: 10.1016/s0022-5347(17)38447-1. https://www.ncbi.
nlm.nih.gov/pubmed/2005698
Gelbard M.K., James K., Riach P., Dorey F.: Collagenase versus placebo in the
treatment of Peyronie’s disease: a double-blind study. J Urol. 1993, 149 (1),
56–58. doi: 10.1016/s0022-5347(17)35998-0. https://www.ncbi.nlm.nih.
gov/pubmed/8417217
Gennaro R., Barletta D., Paulis G.: Intralesional hyaluronic acid: an innovative treatment for Peyronie’s disease. Int Urol Nephrol. 2015, 47 (10),
1595–1602. doi: 10.1007/s11255-015-1074-1. https://www.ncbi.nlm.nih.
gov/pubmed/26257044
Ghanem H.M., Salonia A., Martin-Morales A.: SOP: physical examination and
laboratory testing for men with erectile dysfunction. J Sex Med. 2013, 10
(1), 108–110. doi: 10.1111/j.1743-6109.2012.02734.x. https://www.ncbi.
nlm.nih.gov/pubmed/22524416
Gholami S.S., Lue T.F.: Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol. 2002. 167 (5), 2066–2069.
https://www.ncbi.nlm.nih.gov/pubmed/11956440
Giannetta E., Feola T., Gianfrilli D., Pofi R., Dall’Armi V., Badagliacca R. i wsp.:
Is chronic inhibition of phosphodiesterase type 5 cardioprotective and
safe? A meta-analysis of randomized controlled trials. BMC Med. 2014,
12, 185. doi: 10.1186/s12916-014-0185-3. https://www.ncbi.nlm.nih.gov/
pubmed/25330139
Gittelman M., McMahon C.G., Rodríguez-Rivera J.A., Beneke M., Ulbrich E., Ewald
S.: The POTENT II randomised trial: efficacy and safety of an orodispersible vardenafil formulation for the treatment of erectile dysfunction. Int J
Clin Pract. 2010, 64 (5), 594–603. doi: 10.1111/j.1742-1241.2010.02358.x.
https://www.ncbi.nlm.nih.gov/pubmed/20456213
Giuliano F.: 5-Hydroxytryptamine in premature ejaculation: opportunities for therapeutic intervention. Trends Neurosci. 2007, 30 (2),
79–84. doi: 10.1016/j.tins.2006.12.002. https://www.ncbi.nlm.nih.gov/
pubmed/17169440
Giuliano F., Jackson G., Montorsi F., Martin-Morales A., Raillard P.: Safety of
sildenafil citrate: review of 67 double-blind placebo-controlled trials and
the postmarketing safety database. Int J Clin Pract. 2010, 64 (2), 240–255.
doi: 10.1111/j.1742-1241.2009.02254.x. https://www.ncbi.nlm.nih.gov/
pubmed/19900167
Giuliano F., Patrick D.L., Porst H., La Pera G., Kokoszka A., Merchant S. i wsp.:
Premature ejaculation: results from a five-country European observational
study. Eur Urol. 2008, 53 (5), 1048–1057. doi: 10.1016/j.eururo.2007.10.015.
https://www.ncbi.nlm.nih.gov/pubmed/17950985
Glickman L., Godoy G., Lepor H.: Changes in continence and erectile function between 2 and 4 years after radical prostatectomy. J Urol. 2009, 181
(2), 731–735. doi: 10.1016/j.juro.2008.10.019. https://www.ncbi.nlm.nih.
gov/pubmed/19091349
Glina F.P., de Freitas Barboza J.W., Nunes V.M., Glina S., Bernardo W.M.: What
Is the Impact of Bariatric Surgery on Erectile Function? A Systematic Review
and Meta-Analysis. Sex Med Rev. 2017, 5 (3), 393–402. doi: 10.1016/j.
sxmr.2017.03.008. https://www.ncbi.nlm.nih.gov/pubmed/28526630
Glina S., Ghanem H.: SOP: corpus cavernosum assessment (cavernosography/
cavernosometry). J Sex Med. 2013, 10 (1), 111–114. doi: 10.1111/j.1743-
6109.2012.02795.x. https://www.ncbi.nlm.nih.gov/pubmed/22971225
Glina S., Sharlip I.D., Hellstrom W.J.: Modifying risk factors to prevent and treat
erectile dysfunction. J Sex Med. 2013, 10 (1), 115–119. doi: 10.1111/j.1743-
6109.2012.02816.x. https://www.ncbi.nlm.nih.gov/pubmed/22971247
Goldstein I., Lue T.F., Padma-Nathan H., Rosen R.C., Steers W.D., Wicker
P.A.: Oral sildenafil in the treatment of erectile dysfunction. Sildenafil
Study Group. N Engl J Med. 1998, 338 (20), 1397–1404. doi: 10.1056/
NEJM199805143382001. https://www.ncbi.nlm.nih.gov/pubmed/9580646
Goldstein I., Lue T.F., Padma-Nathan H., Rosen R.C., Steers W.D., Wicker P.A.:
Oral sildenafil in the treatment of erectile dysfunction. 1998. J Urol. 2002,
167, 1197–1203. doi: 10.1016/s0022-5347(02)80386-x. https://www.ncbi.
nlm.nih.gov/pubmed/11905901
Goldstein I., McCullough A.R., Jones L.A., Hellstrom W.J., Bowden C.H., Didonato
K. i wsp.: A randomized, double-blind, placebo-controlled evaluation of the
safety and efficacy of avanafil in subjects with erectile dysfunction. J Sex
Med. 2012, 9 (4), 1122–1133. doi: 10.1111/j.1743-6109.2011.02629.x.
https://www.ncbi.nlm.nih.gov/pubmed/22248153
Goldstein I., Tseng L.J., Creanga D., Stecher V., Kaminetsky J.C.: Efficacy and
Safety of Sildenafil by Age in Men With Erectile Dysfunction. J Sex Med.
2016, 13 (5), 852–859. doi: 10.1016/j.jsxm.2016.02.166. https://www.ncbi.
nlm.nih.gov/pubmed/27114196
Gonzalez-Cadavid N.F., Rajfer J.: Mechanisms of Disease: new insights into
the cellular and molecular pathology of Peyronie’s disease. Nat Clin Pract
Urol. 2005, 2 (6), 291–297. doi: 10.1038/ncpuro0201. https://www.ncbi.
nlm.nih.gov/pubmed/16474811
Gorich J., Ermis C., Krämer S.C., Fleiter T., Wisianowsky C., Basche S. i wsp.:
Interventional treatment of traumatic priapism. J Endovasc Ther. 2002, 9
(5), 614–617. doi: 10.1177/152660280200900511. https://www.ncbi.nlm.
nih.gov/pubmed/12431145
Gratzke C., Angulo J., Chitaley K., Dai Y.T., Kim N.N., Paick J.S. i wsp.: Anatomy,
physiology, and pathophysiology of erectile dysfunction. J Sex Med. 2010,
7, 445–475. doi: 10.1111/j.1743-6109.2009.01624.x. https://www.ncbi.
nlm.nih.gov/pubmed/20092448
Grayhack J.T., McCullough W., O’Conor V.J. Jr, Trippel O.: Venous bypass to
control priapism. Invest Urol. 1964, 1, 509–513. https://www.ncbi.nlm.
nih.gov/pubmed/14130594
Greco E.A., Spera G., Aversa A.: Combining testosterone and PDE5 inhibitors in erectile dysfunction: basic rationale and clinical evidences. Eur Urol.
2006, 50 (3), 940–947. doi: 10.1016/j.eururo.2006.06.049. https://www.
ncbi.nlm.nih.gov/pubmed/16979814
Greenfield J.M., Lucas S., Levine L.A.: Factors affecting the loss of length
associated with tunica albuginea plication for correction of penile curvature. J Urol, 2006, 175 (1), 238–241. doi: 10.1016/S0022-5347(05)00063-
7. https://www.ncbi.nlm.nih.gov/pubmed/16406919
Greenfield J.M., Shah S.J., Levine LA.: Verapamil versus saline in electromotive drug administration for Peyronie’s disease: a double-blind, placebo controlled trial. J Urol. 2007, 177 (3), 972–975. doi: 10.1016/j.juro.2006.10.065.
https://www.ncbi.nlm.nih.gov/pubmed/17296390
Grenier G., Byers E.S.: Rapid ejaculation: a review of conceptual, etiological,
and treatment issues. Arch Sex Behav. 1995, 24 (2), 447–472. doi: 10.1007/
bf01541858. https://www.ncbi.nlm.nih.gov/pubmed/7661658
Griffiths M.R., Priestley G.C.: A comparison of morphoea and lichen sclerosus et atrophicus in vitro: the effects of para-aminobenzoate on skin fibroblasts. Acta Derm Venereol. 1992, 72 (1), 15–18. https://www.ncbi.nlm.
nih.gov/pubmed/1350132
Gross M.S., Phillips E.A., Balen A., Eid J.F., Yang C., Simon R. i wsp.: The
Malleable Implant Salvage Technique: Infection Outcomes after Mulcahy
Salvage Procedure and Replacement of Infected Inflatable Penile Prosthesis
with Malleable Prosthesis. J Urol. 2016, 195 (3), 694–697. doi: 10.1016/j.
juro.2015.08.091. https://www.ncbi.nlm.nih.gov/pubmed/26343986
Gruenwald I., Appel B., Kitrey N.D., Vardi Y.: Shockwave treatment of erectile dysfunction. Ther Adv Urol. 2013, 5 (2), 95–99. doi: 10.1177/1756287212470696.
https://www.ncbi.nlm.nih.gov/pubmed/23554844
Gruenwald I., Appel B., Vardi Y.: Low-intensity extracorporeal shock wave
therapy – a novel effective treatment for erectile dysfunction in severe ED
patients who respond poorly to PDE5 inhibitor therapy. J Sex Med. 2012,
9 (1), 259–264. doi: 10.1111/j.1743-6109.2011.02498.x. https://www.ncbi.
nlm.nih.gov/pubmed/22008059
Gruenwald I., Shenfeld O., Chen J., Raviv G., Richter S., Cohen A. i wsp.: Positive
effect of counseling and dose adjustment in patients with erectile dysfunction who failed treatment with sildenafil. Eur Urol. 2006, 50 (1), 134–
140. doi: 10.1016/j.eururo.2006.01.042. https://www.ncbi.nlm.nih.gov/
pubmed/16527391
Gupta A., Seth T., Gupta A.: Successful use of terbutaline in persistent priapism in a 12-year-old boy with chronic myeloid leukemia. Pediatr Hematol
Oncol. 2009, 26 (1), 70–73. doi: 10.1080/08880010802435146. https://
www.ncbi.nlm.nih.gov/pubmed/19206011
Gupta B.P., Murad M.H., Clifton M.M., Prokop L., Nehra A., Kopecky S.L.: The
effect of lifestyle modification and cardiovascular risk factor reduction on
erectile dysfunction: a systematic review and meta-analysis. Arch Intern
Med. 2011, 171 (20), 1797–1803. doi: 10.1001/archinternmed.2011.440.
https://www.ncbi.nlm.nih.gov/pubmed/21911624
Gupta R., Kirschen J., Barrow R.C. 2nd, Eid J.F.: Predictors of success and risk
factors for attrition in the use of intracavernous injection. J Urol. 1997, 157
(5), 1681–1686. https://www.ncbi.nlm.nih.gov/pubmed/9112505
Gupta S., Salimpour P., Saenz de Tejada I., Daley J., Gholami S., Daller M. i wsp.:
A possible mechanism for alteration of human erectile function by digoxin:
inhibition of corpus cavernosum sodium/potassium adenosine triphosphatase activity. J Urol. 1998, 159 (5), 1529–1536. doi: 10.1097/00005392-
199805000-00033. https://www.ncbi.nlm.nih.gov/pubmed/9554348
Gur S., Limin M., Hellstrom W.J.: Current status and new developments
in Peyronie’s disease: medical, minimally invasive and surgical treatment options. Expert Opin Pharmacother. 2011, 12 (6), 931–944. doi:
10.1517/14656566.2011.544252. https://www.ncbi.nlm.nih.gov/
pubmed/21405946
Guyatt G.H., Oxman A.D., Kunz R., Falck-Ytter Y., Vist G.E., Liberati A. i wsp.:
Going from evidence to recommendations. BMJ. 2008, 336, 1049–1051.
doi: 10.1136/bmj.39493.646875.AE. https://www.ncbi.nlm.nih.gov/
pubmed/18467413
Guyatt G.H., Oxman A.D., Kunz R., Vist G.E., Falck-Ytter Y., Schünemann H.J.:
What is “quality of evidence” and why is it important to clinicians? BMJ.
2008, 336, 995–998. doi: 10.1136/bmj.39490.551019.BE. https://www.
ncbi.nlm.nih.gov/pubmed/18456631
Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P.
i wsp.: GRADE: an emerging consensus on rating quality of evidence and
strength of recommendations. BMJ. 2008, 336, 924–926. doi: 10.1136/
bmj.39489.470347.AD. https://www.ncbi.nlm.nih.gov/pubmed/18436948
Habous M., Farag M., Williamson B., Laban O., Mahmoud S., Abdelwahab
O. i wsp.: Conservative Therapy is an Effective Option in Patients With
Localized Infection After Penile Implant Surgery. J Sex Med. 2016, 13 (6),
972–975. doi: 10.1016/j.jsxm.2016.04.064. https://www.ncbi.nlm.nih.gov/
pubmed/27162191
Haddad R.M., Kennedy C.C., Caples S.M., Tracz M.J., Boloña E.R., Sideras K.
i wsp.: Testosterone and cardiovascular risk in men: a systematic review and
meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc.
2007, 82 (1), 29–39. doi: 10.4065/82.1.29. https://www.ncbi.nlm.nih.gov/
pubmed/17285783
Haglind E., Carlsson S., Stranne J., Wallerstedt A., Wilderäng U., Thorsteinsdottir
T. i wsp.: Urinary Incontinence and Erectile Dysfunction after Robotic Versus
Open Radical Prostatectomy: A Prospective, Controlled, Nonrandomised
Trial. Eur Urol. 2015, 68 (2), 216–225. doi: 10.1016/j.eururo.2015.02.029.
https://www.ncbi.nlm.nih.gov/pubmed/25770484
Hakim L.S., Kulaksizoglu H., Mulligan R., Greenfield A., Goldstein I.: Evolving
concepts in the diagnosis and treatment of arterial high flow priapism. J Urol.
1996, 155 (2), 541–548. https://www.ncbi.nlm.nih.gov/pubmed/8558656
Hanafy H.M., Saad S.M., Al-Ghorab M.M.: Ancient Egyptian medicine: contribution to urology. Urology. 1974, 4 (1), 114–120. doi: 10.1016/0090-
4295(74)90124-1. https://www.ncbi.nlm.nih.gov/pubmed/21323001
Hatzichristodoulou G., Gschwend J.E., Lahme S.: Surgical therapy of Peyronie’s
disease by partial plaque excision and grafting with collagen fleece: feasibility study of a new technique. Int J Impot Res. 2013, 25 (5), 183–187. doi:
10.1038/ijir.2013.7. https://www.ncbi.nlm.nih.gov/pubmed/23446807
Hatzichristou D., Kirana P.S., Banner L., Althof S.E., Lonnee-Hoffmann R.A.,
Dennerstein L.: Diagnosing Sexual Dysfunction in Men and Women: Sexual
History Taking and the Role of Symptom Scales and Questionnaires. J Sex
Med. 2016, 13 (8), 1166–1182. doi: 10.1016/j.jsxm.2016.05.017. https://
www.ncbi.nlm.nih.gov/pubmed/27436074
Hatzichristou D., Moysidis K., Apostolidis A., Bekos A., Tzortzis V., Hatzimouratidis
K. i wsp.: Sildenafil failures may be due to inadequate patient instructions
and follow-up: a study on 100 non-responders. Eur Urol. 2005, 47 (4), 518–
522. doi: 10.1016/j.eururo.2004.12.005. https://www.ncbi.nlm.nih.gov/
pubmed/15774252
Hatzichristou D., Rosen R.C., Derogatis L.R., Low W.Y., Meuleman E.J., Sadovsky
R. i wsp.: Recommendations for the clinical evaluation of men and women
with sexual dysfunction. J Sex Med. 2010, 7, 337–348. doi: 10.1111/j.1743-
6109.2009.01619.x. https://www.ncbi.nlm.nih.gov/pubmed/20092443
Hatzichristou D., Salpiggidis G., Hatzimouratidis K., Apostolidis A., Tzortzis V.,
Bekos A.: Management strategy for arterial priapism: therapeutic dilemmas.
J Urol. 2002, 168 (2), 2074–2077. doi: 10.1097/01.ju.0000032743.39599.
ae. https://www.ncbi.nlm.nih.gov/pubmed/12394712
Hatzichristou D., Hatzimouratidis K., Apostolidis A., Ioannidis E., Yannakoyorgos
K., Kalinderis A.: Hemodynamic characterization of a functional erection.
Arterial and corporeal veno-occlusive function in patients with a positive intracavernosal injection test. Eur Urol. 1999, 36 (1), 60–67. doi:
10.1159/000019928. https://www.ncbi.nlm.nih.gov/pubmed/10364657
Hatzichristou D., Hatzimouratidis K., Apostolidis A., Tzortzis V., Bekos A., Ioannidis
E.: Corporoplasty using tunica albuginea free grafts for penile curvature:
surgical technique and long-term results. J Urol. 2002, 167 (3), 1367–1370.
https://www.ncbi.nlm.nih.gov/pubmed/11832734
Hatzichristou D., Hatzimouratidis K., Ioannides E., Yannakoyorgos K., Dimitriadis
G., Kalinderis A.: Nocturnal penile tumescence and rigidity monitoring in
young potent volunteers: reproducibility, evaluation criteria and the effect
of sexual intercourse. J Urol. 1998, 159 (6), 1921–1926. https://www.ncbi.
nlm.nih.gov/pubmed/9598488
Hatzimouratidis K., Amar E., Eardley I., Giuliano F., Hatzichristou D., Montorsi
F. i wsp.: Guidelines on male sexual dysfunction: erectile dysfunction and
premature ejaculation. Eur Urol. 2010, 57 (5), 804–814. doi: 10.1016/j.
eururo.2010.02.020. https://www.ncbi.nlm.nih.gov/pubmed/20189712
Hatzimouratidis K., Eardley I., Giuliano F., Hatzichristou D., Moncada I., Salonia
A. i wsp.: EAU guidelines on penile curvature. Eur Urol. 2012, 62 (3), 543–
552. doi: 10.1016/j.eururo.2012.05.040. https://www.ncbi.nlm.nih.gov/
pubmed/22658761
Hatzimouratidis K., Giuliano F., Moncada I., Muneer A., Salonia A., Verze P.:
EAU Guidelines Panel on Male Sexual Dysfunction. EAU guidelines on
Penile Curvature. Edn. presented at the EAU Annual Congress Paris. 2012:
Arnhem, The Netherlands. http://uroweb.org/guideline/penile-curvature/
Hatzimouratidis K., Giuliano F., Moncada I., Muneer A., Salonia A., Verze P.:
Guideline Associates: A. Parnham, E.C. Serefogluet al., EAU Guidelines Panel
on Male Sexual Dysfunction. EAU guidelines on Male Sexual Dysfunction.
Edn. presented at the EAU Annual Congress Munich 2016. http://uroweb.
org/guideline/male-sexual-dysfunction/
Hatzimouratidis K., Moysidis K., Bekos A., Tsimtsiou Z., Ioannidis E., Hatzichristou
D.: Treatment strategy for “non-responders” to tadalafil and vardenafil: a real-life study. Eur Urol. 2006, 50 (1), 126–132. doi: 10.1016/j.
eururo.2006.02.060. https://www.ncbi.nlm.nih.gov/pubmed/16564127
Hatzimouratidis K., Salonia A., Adaikan G., Buvat J., Carrier S., El-Meliegy A.
i wsp.: Pharmacotherapy for Erectile Dysfunction: Recommendations From
the Fourth International Consultation for Sexual Medicine (ICSM 2015). J
Sex Med. 2016, 13 (4), 465–488. doi: 10.1016/j.jsxm.2016.01.016. https://
www.ncbi.nlm.nih.gov/pubmed/27045254
Hauck E.W., Hauptmann A., Bschleipfer T., Schmelz H.U., Altinkilic B.M., Weidner
W.: Questionable efficacy of extracorporeal shock wave therapy for Peyronie’s
disease: results of a prospective approach. J Urol. 2004, 171 (1), 296–299.
doi: 10.1097/01.ju.0000099891.68488.4e. https://www.ncbi.nlm.nih.gov/
pubmed/14665898
Hawton K., Catalan J., Martin P., Fagg J.: Long-term outcome of sex therapy.
Behav Res Ther. 1986, 24 (6), 665–675. doi: 10.1016/0005-7967(86)90062-
8. https://www.ncbi.nlm.nih.gov/pubmed/3800838
Hayashi Y., Kojima Y., Mizuno K., Tozawa K., Sasaki S., Kohri K.: Modified technique of dorsal plication for penile curvature with or without hypospadias.
Urology. 2002, 59 (4), 584–586. doi: 10.1016/s0090-4295(02)01555-8.
https://www.ncbi.nlm.nih.gov/pubmed/11927319
Heidenreich A., Bastian P.J., Bellmunt J., Bolla M., Joniau S., van der Kwast T.
i wsp.: EAU guidelines on prostate cancer. part 1: screening, diagnosis, and
local treatment with curative intent-update 2013. Eur Urol. 2014, 65 (1),
124–137. doi: 10.1016/j.eururo.2013.09.046. https://www.ncbi.nlm.nih.
gov/pubmed/24207135
Hellstrom W.J., Bivalacqua T.J.: Peyronie’s disease: etiology, medical, and
surgical therapy. J Androl. 2000, 21 (3), 347–354. https://www.ncbi.nlm.
nih.gov/pubmed/10819440
Hellstrom W.J., Feldman R.A., Coyne K.S., Kaufman G.J., Smith T.M., Tursi J.P.
i wsp.: Self-report and Clinical Response to Peyronie’s Disease Treatment:
Peyronie’s Disease Questionnaire Results From 2 Large Double-Blind,
Randomized, Placebo-Controlled Phase 3 Studies. Urology. 2015, 86 (2),
291–298. doi: 10.1016/j.urology.2015.04.047. https://www.ncbi.nlm.nih.
gov/pubmed/26199168
Hellstrom W.J., Feldman R., Rosen R.C., Smith T., Kaufman G., Tursi J.: Bother
and distress associated with Peyronie’s disease: validation of the Peyronie’s
disease questionnaire. J Urol. 2013, 190 (2), 627–634. doi: 10.1016/j.
juro.2013.01.090. https://www.ncbi.nlm.nih.gov/pubmed/23376705
Hellstrom W.J., Kaminetsky J., Belkoff L.H., Goldstein I., Tursi J.P., Uy J.
i wsp.: Efficacy of Avanafil 15 Minutes after Dosing in Men with Erectile
Dysfunction: A Randomized, Double-Blind, Placebo Controlled Study. J
Urol. 2015, 194 (2), 485–492. doi: 10.1016/j.juro.2014.12.101. https://www.
ncbi.nlm.nih.gov/pubmed/25591992
Hellstrom W.J., Kendirci M., Matern R., Cockerham Y., Myers L., Sikka S.C.
i wsp.: Single-blind, multicenter, placebo controlled, parallel study to assess
the safety and efficacy of intralesional interferon alpha-2B for minimally
invasive treatment for Peyronie’s disease. J Urol. 2006, 176 (1), 394–398.
doi: 10.1016/S0022-5347(06)00517-9. https://www.ncbi.nlm.nih.gov/
pubmed/16753449
Hellstrom W.J., Montague D.K., Moncada I., Carson C., Minhas S., Faria G. i wsp.:
Implants, mechanical devices, and vascular surgery for erectile dysfunction. J Sex Med. 2010, 7, 501–523. doi: 10.1111/j.1743-6109.2009.01626.x.
https://www.ncbi.nlm.nih.gov/pubmed/20092450
Henry G.D., Brinkman M.J., Mead S.F., Delk J.R. 2nd, Cleves M.A., Jennermann
C. i wsp.: A survey of patients with inflatable penile prostheses: assessment
of timing and frequency of intercourse and analysis of implant durability. J
Sex Med. 2012, 9 (6), 1715–1721. doi: 10.1111/j.1743-6109.2012.02729.x.
https://www.ncbi.nlm.nih.gov/pubmed/22568579
Henry G.D., Donatucci C.F., Conners W., Greenfield J.M., Carson C.C., Wilson
S.K. i wsp.: An outcomes analysis of over 200 revision surgeries for penile
prosthesis implantation: a multicenter study. J Sex Med. 2012, 9 (1), 309–
315. doi: 10.1111/j.1743-6109.2011.02524.x. https://www.ncbi.nlm.nih.
gov/pubmed/22082149
Hisasue S., China T., Horiuchi A., Kimura M., Saito K., Isotani S. i wsp.: Impact
of aging and comorbidity on the efficacy of low-intensity shock wave therapy for erectile dysfunction. Int J Urol. 2016, 23 (1), 80–84. doi: 10.1111/
iju.12955. https://www.ncbi.nlm.nih.gov/pubmed/26501992
Hoyerup P., Azawi N.H.: Partial priapism. BMJ Case Rep. 2013, 2013.
doi: 10.1136/bcr-2013-200031. https://www.ncbi.nlm.nih.gov/
pubmed/23933863
Hsu C.Y., Lin C.L., Kao C.H.: Gout is associated with organic and psychogenic
erectile dysfunction. Eur J Intern Med. 2015, 26 (9), 691–695. doi: 10.1016/j.
ejim.2015.06.001. https://www.ncbi.nlm.nih.gov/pubmed/26089189
Hubler J., Szanto A., Konyves K.: Methylene blue as a means of treatment for priapism caused by intracavernous injection to combat erectile dysfunction. Int
Urol Nephrol. 2003, 35 (4), 519–521. doi: 10.1023/b:urol.0000025617.97048.
ae. https://www.ncbi.nlm.nih.gov/pubmed/15198160
Husain J., Lynn N.N., Jones D.K., Collins G.N., O’Reilly P.H.: Extracorporeal
shock wave therapy in the management of Peyronie’s disease: initial experience. BJU Int. 2000, 86 (4), 466–468. doi: 10.1046/j.1464-
410x.2000.00827.x. https://www.ncbi.nlm.nih.gov/pubmed/10971273
Ilkay A.K., Levine L.A.: Conservative management of high-flow priapism. Urology. 1995, 46 (3), 419–424. https://www.ncbi.nlm.nih.gov/
pubmed/7660524
Inamoto T., Azuma H., Iwamoto Y., Sakamoto T., Katsuoka Y.A.: rare case of penile
metastasis of testicular cancer presented with priapism. Hinyokika Kiyo.
2005, 51 (9), 639–642. https://www.ncbi.nlm.nih.gov/pubmed/16229380
Incrocci L., Jensen P.T.: Pelvic radiotherapy and sexual function in men and
women. J Sex Med. 2013, 10 Suppl 1, 53–64. doi: 10.1111/jsm.12010. https://
www.ncbi.nlm.nih.gov/pubmed/23387912
Isgoren A., Saitz T.R., Serefoglu E.C.: Erectile function outcomes after robotassisted radical prostatectomy: is it superior to open retropubic or laparoscopic approach? Sex Med Rev. 2014, 2 (2), 20–23. doi: 10.1002/smrj.21.
https://www.ncbi.nlm.nih.gov/pubmed/27784540
Isidori A.M., Buvat J., Corona G., Goldstein I., Jannini E.A., Lenzi A. i wsp.:
A critical analysis of the role of testosterone in erectile function: from
pathophysiology to treatment-a systematic review. Eur Urol. 2014, 65 (1),
99–112. doi: 10.1016/j.eururo.2013.08.048. https://www.ncbi.nlm.nih.
gov/pubmed/24050791
Jackson G.: Hemodynamic and exercise effects of phosphodiesterase 5 inhibitors. Am J Cardiol. 2005, 96, 32M–36M. doi: 10.1016/j.amjcard.2005.07.009.
https://www.ncbi.nlm.nih.gov/pubmed/16387564
Jackson G., Montorsi P., Adams M.A., Anis T., El-Sakka A., Miner M. i wsp.:
Cardiovascular aspects of sexual medicine. J Sex Med. 2010, 7, 1608–1626.
doi: 10.1111/j.1743-6109.2010.01779.x. https://www.ncbi.nlm.nih.gov/
pubmed/20388161
Jarow J.P., Lowe F.C.: Penile trauma: an etiologic factor in Peyronie’s disease
and erectile dysfunction. J Urol. 1997, 158 (4), 1388–1390. doi: 10.1016/
s0022-5347(01)64222-8. https://www.ncbi.nlm.nih.gov/pubmed/9302127
Ji S., Zang Z., Ma H., Gu M., Han Y., Wang L. i wsp.: Erectile dysfunction in
patients with plaque psoriasis: the relation of depression and cardiovascular factors. Int J Impot Res. 2016, 28 (3), 96–100. doi: 10.1038/ijir.2016.6.
https://www.ncbi.nlm.nih.gov/pubmed/26865100
Johannes C.B., Araujo A.B., Feldman H.A., Derby C.A., Kleinman K.P., McKinlay
J.B.: Incidence of erectile dysfunction in men 40 to 69 years old: longitudinal results from the Massachusetts male aging study. J Urol. 2000, 163 (2),
460–463. https://www.ncbi.nlm.nih.gov/pubmed/10647654
Jordan G.H.: The use of intralesional clostridial collagenase injection
therapy for Peyronie’s disease: a prospective, single-center, non-placebocontrolled study. J Sex Med. 2008, 5 (1), 180–187. doi: 10.1111/j.1743-
6109.2007.00651.x. https://www.ncbi.nlm.nih.gov/pubmed/18173766
Junemann K.P., Persson-Jünemann C., Alken P.: Pathophysiology of erectile
dysfunction. Semin Urol. 1990, 8 (2), 80–93. https://www.ncbi.nlm.nih.
gov/pubmed/2191403
Kadioglu A., Akman T., Sanli O., Gurkan L., Cakan M., Celtik M. i wsp.: Surgical
treatment of Peyronie’s disease: a critical analysis. Eur Urol. 2006, 50 (2),
235–248. doi: 10.1016/j.eururo.2006.04.030. https://www.ncbi.nlm.nih.
gov/pubmed/16716495
Kadioglu A., Tefekli A., Erol H., Cayan S., Kandirali E.: Color Doppler ultrasound
assessment of penile vascular system in men with Peyronie’s disease. Int
J Impot Res. 2000, 12 (5), 263–267. doi: 10.1038/sj.ijir.3900569. https://
www.ncbi.nlm.nih.gov/pubmed/11424963
Kadioglu A., Tefekli A., Erol B., Oktar T., Tunc M., Tellaloglu S.: A retrospective
review of 307 men with Peyronie’s disease. J Urol. 2002, 168 (3), 1075–
1079. doi: 10.1097/01.ju.0000024040.55662.36. https://www.ncbi.nlm.
nih.gov/pubmed/12187226
Kadioglu A., Tefekli A., Köksal T., Usta M., Erol H.: Treatment of Peyronie’s
disease with oral colchicine: long-term results and predictive parameters of
successful outcome. Int J Impot Res. 2000, 12 (3), 169–175. doi: 10.1038/
sj.ijir.3900519. https://www.ncbi.nlm.nih.gov/pubmed/11045911
Kadioglu A., Tefekli A., Usta M., Demirel S., Tellaloğlu S.: Surgical treatment of
Peyronie’s disease with incision and venous patch technique. Int J Impot
Res. 1999, 11 (2), 75–81. doi: 10.1038/sj.ijir.3900375. https://www.ncbi.
nlm.nih.gov/pubmed/10356666
Kandel G.L., Bender L.I., Grove J.S.: Pulmonary embolism: a complication
of corpus-saphenous shunt for priapism. J Urol. 1968, 99 (2), 196–197.
doi: 10.1016/s0022-5347(17)62672-7. https://www.ncbi.nlm.nih.gov/
pubmed/5641077
Kang B.C., Lee D.Y., Byun J.Y., Baek S.Y., Lee S.W., Kim K.W.: Post-traumatic
arterial priapism: colour Doppler examination and superselective arterial
embolization. Clin Radiol. 1998, 53 (11), 830–834. doi: 10.1016/s0009-
9260(98)80195-5. https://www.ncbi.nlm.nih.gov/pubmed/9833787
Kao C.C., Lin C.L., Huang W.Y., Cha T.L., Lin T.Y., Shen C.H. i wsp.: Association
Between Inflammatory Bowel Disease and Erectile Dysfunction: A
Nationwide Population-Based Study. Inflamm Bowel Dis. 2016, 22 (5),
1065–1070. doi: 10.1097/MIB.0000000000000695. https://www.ncbi.
nlm.nih.gov/pubmed/26863266
Karagiannis A.A., Sopilidis O.T., Brountzos E., Staios D.N., Kelekis N.L., Kelekis
D.A.: High flow priapism secondary to internal urethrotomy treated
with embolization. J Urol. 2004, 171 (4), 1631–1632. doi: 10.1097/01.
ju.0000116287.03211.8d. https://www.ncbi.nlm.nih.gov/pubmed/15017242
Kato G.J.: Priapism in sickle-cell disease: a hematologist’s perspective. J Sex
Med. 2012, 9 (1), 70–78. doi: 10.1111/j.1743-6109.2011.02287.x. https://
www.ncbi.nlm.nih.gov/pubmed/21554552
Keating G.M., Scott L.J.: Vardenafil: a review of its use in erectile dysfunction.
Drugs. 2003, 63 (23), 2673–2703. doi: 10.2165/00003495-200363230-
00010. https://www.ncbi.nlm.nih.gov/pubmed/14636086
Kempeneers P., Andrianne R., Bauwens S., Georis I., Pairoux J.F., Blairy S.:
Functional and psychological characteristics of belgian men with premature ejaculation and their partners. Arch Sex Behav. 2013, 42 (1),
51–66. doi: 10.1007/s10508-012-9958-y. https://www.ncbi.nlm.nih.gov/
pubmed/22695640
Kendirci M., Hellstrom W.J.: Critical analysis of surgery for Peyronie’s disease.
Curr Opin Urol. 2004, 14 (6), 381–388. doi: 10.1097/00042307-200411000-
00015. https://www.ncbi.nlm.nih.gov/pubmed/15626883
Kendirci M., Usta M.F., Matern R.V., Nowfar S., Sikka S.C., Hellstrom W.J.:
The impact of intralesional interferon alpha-2b injection therapy on penile
hemodynamics in men with Peyronie’s disease. J Sex Med. 2005, 2 (5),
709–715. doi: 10.1111/j.1743-6109.2005.00110.x. https://www.ncbi.nlm.
nih.gov/pubmed/16422829
Kerlan R.K., Gordon R.L., LaBerge J.M., Ring E.J.: Superselective microcoil
embolization in the management of high-flow priapism. J Vasc Interv Radiol.
1998, 9, 85–89. doi: 10.1016/s1051-0443(98)70488-9. https://www.ncbi.
nlm.nih.gov/pubmed/9468400
Keskin D., Cal C., Delibaş M., Ozyurt C., Günaydin G., Nazli O. i wsp.:
Intracavernosal adrenalin injection in priapism. Int J Impot Res. 2000,
12 (6), 312–314. doi: 10.1038/sj.ijir.3900539. https://www.ncbi.nlm.nih.
gov/pubmed/11416834
Khera M., Adaikan G., Buvat J., Carrier S., El-Meliegy A., Hatzimouratidis K. i wsp.:
Diagnosis and Treatment of Testosterone Deficiency: Recommendations From
the Fourth International Consultation for Sexual Medicine (ICSM 2015).
J Sex Med. 2016, 13 (12), 1787–1804. doi: 10.1016/j.jsxm.2016.10.009.
https://www.ncbi.nlm.nih.gov/pubmed/27914560
Khera M., Crawford D., Morales A., Salonia A., Morgentaler A.: A new era of
testosterone and prostate cancer: from physiology to clinical implications.
Eur Urol. 2014, 65 (1), 115–123. doi: 10.1016/j.eururo.2013.08.015. https://
www.ncbi.nlm.nih.gov/pubmed/24011426
Khoder W.Y., Waidelich R., Seitz M., Becker A.J., Buchner A., Trittschler S. i wsp.:
Stief CG.Do we need the nerve sparing radical prostatectomy techniques
(intrafascial vs. interfascial) in men with erectile dysfunction? Results of
a single-centre study. World J Urol. 2015, 33 (3), 301–307. doi: 10.1007/
s00345-014-1302-9. https://www.ncbi.nlm.nih.gov/pubmed/24752607
Kihl B., Bratt C.G., Knutsson U., Seeman T.: Priapsim: evaluation of treatment with special reference to saphenocavernous shunting in 26 patients.
Scand J Urol Nephrol. 1980, 14 (1), 1–5. doi: 10.3109/00365598009181182.
https://www.ncbi.nlm.nih.gov/pubmed/7375831
Kim D.J., Hawksworth D.J., Hurwitz L.M., Cullen J., Rosner I.L., Lue T.F. i wsp.:
A prospective, randomized, placebo-controlled trial of on-Demand vs. nightly
sildenafil citrate as assessed by Rigiscan and the international index of
erectile function. Andrology. 2016, 4 (1), 27–32. doi: 10.1111/andr.12118.
https://www.ncbi.nlm.nih.gov/pubmed/26663669
Kim D.S., Yang K.M., Chung H.J., Choi H.M., Choi Y.D., Choi H.K.: AMS 700CX/
CXM inflatable penile prosthesis has high mechanical reliability at longterm follow-up. J Sex Med. 2010, 7, 2602–2607. doi: 10.1111/j.1743-
6109.2010.01801.x. https://www.ncbi.nlm.nih.gov/pubmed/20384938
Kim J.H., Lee H.J., Song Y.S.: Mesenchymal stem cell-based gene therapy for
erectile dysfunction. Int J Impot Res. 2016, 28 (3), 81–87. doi: 10.1038/
ijir.2016.3. https://www.ncbi.nlm.nih.gov/pubmed/26888355
Kim K.R., Shin J.H., Song H.Y., Ko G.Y., Yoon H.K., Sung K.B. i wsp.: Treatment
of high-flow priapism with superselective transcatheter embolization in 27
patients: a multicenter study. J Vasc Interv Radiol. 2007, 18 (10), 1222–
1226. doi: 10.1016/j.jvir.2007.06.030. https://www.ncbi.nlm.nih.gov/
pubmed/17911511
Kim M., Kim S.Y., Rou W.S., Hwang S.W., Lee B.S.: Erectile dysfunction in
patients with liver disease related to chronic hepatitis B. Clin Mol Hepatol.
2015, 21 (4), 352–357. doi: 10.3350/cmh.2015.21.4.352. https://www.ncbi.
nlm.nih.gov/pubmed/26770923
Kim S.W., Paick J.S.: Short-term analysis of the effects of as needed use of
sertraline at 5 PM for the treatment of premature ejaculation. Urology. 1999,
54 (3), 544–547. doi: 10.1016/s0090-4295(99)00187-9. https://www.ncbi.
nlm.nih.gov/pubmed/10475369
Kirby E.W., Carson C.C., Coward R.M.: Tramadol for the management of premature ejaculation: A timely systematic review. Int J Impot Res. 2015,
27 (4), 121–127. doi: 10.1038/ijir.2015.7. https://www.ncbi.nlm.nih.gov/
pubmed/25971856
Kitrey N.D., Gruenwald I., Appel B., Shechter A., Massarwa O., Vardi Y.
i wsp.: Penile Low Intensity Shock Wave Treatment is Able to Shift PDE5i
Nonresponders to Responders: A Double-Blind, Sham Controlled Study. J
Urol. 2016, 195 (5), 1550–1555. doi: 10.1016/j.juro.2015.12.049. https://
www.ncbi.nlm.nih.gov/pubmed/26694904
Kloner R.A., Jackson G., Emmick J.T., Mitchell M.I., Bedding A., Warner M.R.
i wsp.: Interaction between the phosphodiesterase 5 inhibitor, tadalafil and
2 alpha-blockers, doxazosin and tamsulosin in healthy normotensive men.
J Urol. 2004, 172, 1935–1940. doi: 10.1097/01.ju.0000142687.75577.e4.
https://www.ncbi.nlm.nih.gov/pubmed/15540759
Knoll L.D.: Use of porcine small intestinal submucosal graft in the surgical management of Peyronie’s disease. Urology. 2001, 57 (4), 753–757.
doi: 10.1016/s0090-4295(00)01079-7. https://www.ncbi.nlm.nih.gov/
pubmed/11306396
Kolbenstvedt A., Egge T., Schultz A.: Arterial high flow priapism role of radiology in diagnosis and treatment. Scand J Urol Nephrol Suppl. 1996, 179,
143–146. https://www.ncbi.nlm.nih.gov/pubmed/8908681
Kostis J.B., Jackson G., Rosen R., Barrett-Connor E., Billups K., Burnett A.L.
i wsp.: Sexual dysfunction and cardiac risk (the Second Princeton Consensus
Conference). Am J Cardiol. 2005, 96 (2), 313–321. doi: 10.1016/j.amjcard.2005.03.065. https://www.ncbi.nlm.nih.gov/pubmed/16018863
Kovanecz I., Rambhatla A., Ferrini M.G., Vernet D., Sanchez S., Rajfer J. i wsp.:
Chronic daily tadalafil prevents the corporal fibrosis and veno-occlusive
dysfunction that occurs after cavernosal nerve resection. BJU Int. 2008,
101 (2), 203–210. doi: 10.1111/j.1464-410X.2007.07223.x. https://www.
ncbi.nlm.nih.gov/pubmed/17888043
Kropman R.F., Schipper J.: Hematoma or “partial priapism” in the proximal
part of the corpus cavernosum. J Sex Med. 2014, 11 (10), 2618–2622. doi:
10.1111/jsm.12388. https://www.ncbi.nlm.nih.gov/pubmed/24308665
